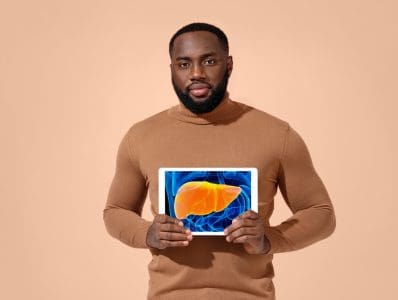
Urination problems affect millions of men worldwide, often developing so gradually that many dismiss early warning signs. Medical experts emphasize that early intervention can prevent complications and lead to better treatment outcomes. Understanding these issues and their solutions has become increasingly important as the global population ages and medical advances offer more effective treatments.
Understanding the basics
The male urinary system’s complexity makes it susceptible to various issues as men age. While some problems resolve naturally, others require medical intervention to prevent long-term complications. Prostate enlargement, known as benign prostatic hyperplasia (BPH), remains the most common cause of urination difficulties in men over 50. This condition develops when the prostate gland gradually enlarges, putting pressure on the urethra and causing various urinary symptoms.
Bladder function changes also play a significant role in urination problems. As men age, the bladder muscle can become either overactive, leading to frequent urination, or underactive, making it difficult to empty the bladder completely. These changes often occur gradually, making it crucial for men to pay attention to subtle changes in their urinary habits.
Urinary tract infections, though less common in men than women, can cause significant discomfort and require prompt treatment. The presence of kidney stones can also disrupt normal urination patterns, sometimes leading to severe pain and urinary blockage. Additionally, neurological conditions affecting bladder control may develop over time, impacting the complex coordination between the brain and urinary system.
Recognition and early detection
Medical professionals emphasize the importance of recognizing early warning signs of urinary problems. Increased urination frequency, particularly at night, often serves as one of the first indicators of developing issues. Men might notice changes in their urine stream strength or experience difficulty starting or stopping urination. A persistent feeling of incomplete bladder emptying can indicate problems with the prostate or bladder function.
Pain or burning during urination should never be ignored, as it could signal an infection or other serious condition. The appearance of blood in urine, while alarming, provides an important warning sign that requires immediate medical attention. These symptoms, especially when occurring together, warrant prompt medical evaluation.
Treatment approaches
Modern medicine offers comprehensive treatment options that extend beyond simple medication. Health care providers typically begin with conservative approaches, gradually moving to more intensive treatments if necessary. Lifestyle modifications often serve as the foundation of treatment, with health care providers recommending scheduled fluid intake management and moderate exercise programs.
Medication remains a cornerstone of treatment for many urinary conditions. Alpha blockers help relax prostate and bladder neck muscles, improving urine flow in BPH cases. Other medications target specific conditions like overactive bladder or chronic inflammation. These treatments often work best when combined with lifestyle changes and regular monitoring.
Minimally invasive procedures have revolutionized the treatment of male urinary problems. Modern surgical techniques allow for precise treatment with reduced recovery times and fewer complications. These procedures can often be performed on an outpatient basis, allowing men to return to their normal activities more quickly.
Impact on daily life
Urinary problems significantly affect quality of life, influencing both physical and emotional well-being. Sleep disruption from nighttime urination can lead to fatigue and decreased daytime productivity. Many men experience anxiety about bathroom access, leading to reduced social activities and workplace challenges. These issues can strain relationships and impact mental health, making comprehensive treatment approaches essential.
Health care professionals now recognize the importance of addressing both physical symptoms and emotional impacts. Support systems, including family understanding and medical team coordination, play crucial roles in successful treatment outcomes. Patient education programs help men understand their conditions and treatment options, leading to better compliance and improved results.
Prevention and ongoing care
Preventive care has become increasingly important in managing male urinary health. Regular screenings after age 40 can detect problems early, when treatment proves most effective. Health care providers recommend maintaining healthy weight through proper diet and exercise, as obesity can exacerbate urinary problems. Proper hydration and avoiding bladder irritants contribute to overall urinary health.
Current medical guidelines suggest annual urological screenings for men over 50, or earlier for those with risk factors or family history. These screenings typically include physical examinations, blood tests, and discussions about urinary symptoms. Early detection through regular screening often leads to simpler, more effective treatments.
Looking forward
Research continues to advance treatment options for male urination issues, offering hope for better outcomes. New medications and minimally invasive procedures emerge regularly, providing more options for treatment. The medical community emphasizes that successful treatment often depends on early intervention, with men who address urinary problems in their early stages typically experiencing better outcomes.
Support systems play a crucial role in treatment success, with family understanding and medical team coordination contributing to better management of urinary health issues. The path to better urinary health starts with awareness and action, empowering men to seek medical evaluation when needed. With current medical advances and growing understanding of male urinary health, effective solutions exist for most urinary problems, particularly when addressed early.
This story was created using AI technology.