The numbers are startling – more than 34 million Americans live with diabetes, but the impact on Black communities tells an even more concerning story. Recent studies show that non-Hispanic Black Americans are facing a diabetes crisis, with rates soaring 60% higher than their non-Hispanic white counterparts. This health disparity has become a critical public health concern, prompting medical professionals and community leaders to take decisive action.
Breaking down the troubling statistics
When looking at the raw data, the disparity becomes crystal clear. Non-Hispanic Black individuals show an 11.7% diabetes prevalence rate, dramatically outpacing the 7.5% rate seen in non-Hispanic white populations. But the story doesn’t end with diagnosis – Black Americans often face more severe complications, including vision loss from diabetic retinopathy and life-threatening kidney problems. The risk of diabetes-related amputations is also significantly higher, with some studies showing rates up to three times higher than those in other populations.
A deeper look at the 5 key factors driving higher diabetes rates
1. Genetic predisposition plays a significant role in diabetes risk for Black Americans. Scientists have identified specific genetic variations, including G6PD deficiency, that may increase susceptibility when combined with environmental factors. Research suggests that these genetic factors may influence how the body processes insulin and regulates blood sugar levels.
2. Limited access to nutritious food options in many predominantly Black neighborhoods creates a significant barrier to maintaining healthy eating habits. These “food deserts” often force residents to rely on processed foods and fast-food options. Studies show that some urban areas with large Black populations have up to 50% fewer supermarkets compared to predominantly white neighborhoods.
3. Economic challenges impact healthcare access and preventive care. Many Black Americans face difficulties affording regular medical check-ups and necessary medications, leading to delayed diagnosis and treatment. The cost of diabetes management, including insulin and blood sugar monitoring supplies, can create an overwhelming financial burden.
4. Chronic stress from systemic inequities takes a physical toll. Research shows that prolonged stress can affect blood sugar levels and contribute to insulin resistance, increasing diabetes risk. This stress often stems from various sources, including workplace discrimination, financial pressures, and environmental concerns.
5. Cultural and environmental factors, including traditional dietary patterns influenced by historical circumstances and limited access to safe outdoor spaces for exercise, can impact overall health outcomes. Many urban areas lack adequate parks, walking trails, or recreational facilities, making it challenging to maintain an active lifestyle.
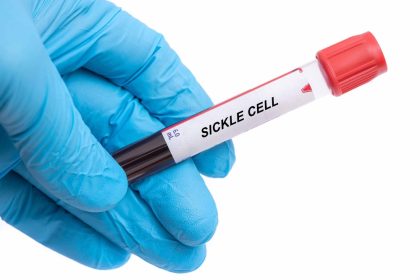
Understanding the disease that’s affecting millions
Diabetes disrupts the body’s ability to properly process glucose, leading to dangerous blood sugar levels. While Type 1 diabetes stems from an autoimmune response, Type 2 diabetes – the more common form – develops when the body becomes resistant to insulin or doesn’t produce enough of this crucial hormone. The condition requires careful management through medication, diet, and lifestyle modifications to prevent serious complications.
Breaking the cycle: Prevention strategies that work
Taking control of diabetes risk starts with awareness and action. Regular medical check-ups, including blood sugar monitoring, serve as the first line of defense. Making sustainable lifestyle changes can significantly reduce the risk of developing Type 2 diabetes.
Successful prevention strategies include maintaining a healthy weight through regular physical activity and balanced nutrition. Even small changes, like taking daily walks or reducing processed food intake, can make a meaningful difference. Community-based programs have shown particular success when they incorporate culturally relevant approaches to diet and exercise.
Resources and support systems making a difference
Across the country, organizations are stepping up to provide crucial support for Black Americans affected by diabetes. These programs offer education, medical resources, and community support networks essential for managing the condition effectively. Local health centers are increasingly offering diabetes prevention programs tailored to the specific needs of Black communities.
From local church health ministries to national advocacy groups, these support systems help individuals navigate their diabetes journey while addressing the unique challenges faced by Black communities. Many organizations now provide virtual support groups, educational workshops, and cooking classes that focus on making traditional recipes healthier without sacrificing cultural significance.
Creating lasting change
The path to reducing diabetes disparities requires a comprehensive approach that addresses both individual health needs and broader systemic issues. Healthcare providers are increasingly recognizing the importance of culturally competent care and developing targeted programs that resonate with Black communities. This includes training medical professionals to better understand and address the specific challenges faced by Black patients.
Progress means acknowledging both the medical and social aspects of diabetes management. By understanding and addressing the complex factors contributing to higher diabetes rates among Black Americans, healthcare providers and community organizations can work together to create more effective solutions. Some healthcare systems have begun implementing innovative programs that combine medical care with social services, addressing both health and socioeconomic factors.
Recent initiatives have shown promising results in reducing diabetes disparities. Community health worker programs, which employ trained individuals from within the community, have been particularly successful in helping people navigate healthcare systems and maintain healthy lifestyles. These programs provide personalized support, helping individuals overcome barriers to care and make sustainable changes in their daily lives.
The fight against diabetes in Black communities continues, but with increased awareness, better resources, and targeted support, positive change is possible. Through understanding these challenges and taking proactive steps, individuals and communities can work together to reduce the impact of this serious health condition. As healthcare systems and community organizations continue to develop more effective interventions, there is hope for reducing the burden of diabetes in Black communities and creating a healthier future for generations to come.