Human papillomavirus (HPV) remains one of the most prevalent viral infections globally, affecting millions across demographics. While many HPV strains pose minimal risk, certain variants can trigger severe health complications, particularly cervical cancer. However, the connection between HPV and ovarian cancer continues to generate scientific discourse and investigation.
Current medical understanding shows no direct causal relationship between HPV and ovarian cancer, though both conditions significantly impact women’s health. Understanding their distinct characteristics, risks, and prevention strategies has become crucial for public health initiatives and individual health care decisions.
The science behind ovarian cancer
Unlike cervical cancer’s clear link to HPV, ovarian cancer develops through multiple pathways. Current research identifies several key risk factors:
- Genetic predisposition, particularly mutations in BRCA1 and BRCA2 genes, substantially increases risk potential, with some women facing up to a 40% lifetime risk of developing ovarian cancer
- Age demographics show higher incidence in women over 50, though cases among younger women continue to emerge, particularly in those with family history
- Reproductive history plays a significant role, including factors such as early menstruation onset, late menopause, and never having given birth
- Environmental and lifestyle influences, from tobacco use to obesity, contribute to overall risk profiles, making lifestyle modifications an important part of prevention
- Hormone replacement therapy may influence risk levels, particularly in post-menopausal women
The complexity of these risk factors underscores the importance of comprehensive health care approaches and regular medical consultations.
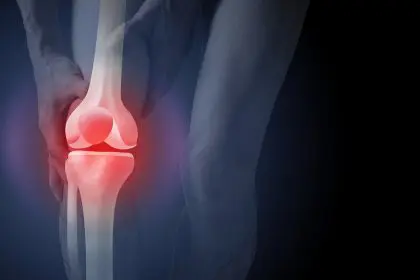
Recognizing early warning signs
Ovarian cancer presents unique diagnostic challenges, often masquerading as common digestive or menstrual issues. This similarity to routine ailments frequently delays crucial early detection. Women should monitor persistent symptoms, including:
- Ongoing bloating or abdominal distention lasting more than two weeks, particularly if it occurs daily or shows no improvement
- Chronic pelvic discomfort or pressure that interferes with daily activities
- Changes in eating patterns or early satiety, including difficulty finishing normal-sized meals
- Increased urinary frequency or urgency that cannot be explained by other conditions
- Unexplained fatigue or weight loss that persists despite lifestyle changes
Medical professionals emphasize that while these symptoms might seem routine, their persistence warrants medical evaluation, particularly if they occur daily for several weeks. The vague nature of these symptoms often contributes to delayed diagnosis, making awareness and proactive health monitoring essential.
Prevention strategies and health management
While no definitive prevention method exists for ovarian cancer, several approaches help reduce risk:
Regular health monitoring remains essential, though standard screening programs like those for cervical cancer don’t exist for ovarian cancer. Women with family histories should discuss genetic testing options with health care providers to understand their individual risk profile and appropriate preventive measures.
Lifestyle modifications play a crucial role in risk reduction. Maintaining healthy body weight through balanced nutrition and regular physical activity contributes to overall cancer prevention strategies. The elimination of tobacco products and limitation of alcohol consumption further supports health maintenance efforts.
Research indicates that oral contraceptive use may reduce ovarian cancer risk, though individual health factors determine suitability. Women considering this option should discuss benefits and potential risks with their health care providers. Some high-risk individuals may consider preventive surgery, particularly those with significant genetic predisposition or family history of ovarian cancer.
The role of HPV vaccination
While HPV vaccination does not prevent ovarian cancer, its importance in women’s health cannot be overlooked. The Centers for Disease Control and Prevention recommends vaccination for:
- Pre-teens aged 11-12, allowing for optimal immune response
- Young adults through age 26 who haven’t been previously vaccinated
- Adults up to age 45 may benefit from vaccination based on individual risk factors and health care provider recommendations
The vaccine’s effectiveness in preventing HPV-related cancers, particularly cervical cancer, makes it a crucial tool in comprehensive women’s health protection.
Dispelling common misconceptions
Clear information helps combat persistent myths about HPV and ovarian cancer. Current medical evidence shows no confirmed direct link between HPV and ovarian cancer, though HPV remains a primary risk factor for cervical and other gynecologic cancers.
The HPV vaccine’s role extends beyond women’s health, with recommendations now including both males and females. This broader approach helps reduce overall disease transmission and impact through community protection.
Diagnostic tools differ significantly between gynecologic cancers. While Pap tests effectively screen for cervical cancer, ovarian cancer requires different detection methods, including ultrasound and blood analysis. Understanding these distinctions helps women better navigate their health care options.
The importance of proactive health care
Regular gynecological examinations remain fundamental to women’s health maintenance. While HPV testing and Pap smears focus on cervical health, comprehensive check-ups allow for broader health discussions and risk assessment.
Health care providers can develop personalized screening and prevention strategies based on individual risk factors. This tailored approach optimizes early intervention opportunities and treatment success rates. Women should maintain open communication with their health care providers about any persistent symptoms or concerns.
Understanding both conditions’ distinct characteristics helps women make informed health decisions. While HPV and ovarian cancer remain separate concerns, awareness of both supports comprehensive women’s health management. Early detection through symptom awareness and regular medical care offers the best opportunity for successful treatment outcomes.
This story was created using AI technology.