Inside the human body, a silent battle rages between diabetes and kidney function, with devastating consequences many never see coming. Recent medical research has uncovered alarming evidence about how elevated blood sugar levels systematically destroy these vital organs, often before patients notice any symptoms.
The intricate filtration dance
The kidneys perform an incredibly complex daily ritual, filtering approximately 150 quarts of blood through millions of microscopic structures called nephrons. These delicate filtering units work tirelessly to remove waste and maintain fluid balance, but diabetes disrupts this careful process in ways researchers are only beginning to understand.
When blood sugar levels remain high, these filtering units sustain progressive damage. Unlike other body tissues that can regenerate, nephrons suffer permanent harm, making prevention absolutely critical for long-term health.
The stark reality
Medical data reveals an unsettling truth – diabetes has emerged as the leading cause of kidney failure worldwide. This devastating condition, known in medical circles as diabetic nephropathy, develops insidiously as persistent high blood sugar levels gradually destroy the intricate network of blood vessels within the kidneys. The damage accumulates silently over years, often detected only after significant harm has occurred.
Breaking the silence
Modern medical screening has revolutionized how doctors detect early kidney damage in diabetes patients. Through sophisticated testing methods, healthcare providers can now identify problems years before obvious symptoms emerge. The urine albumin test serves as an early warning system, detecting minute amounts of protein that signal developing kidney stress. Meanwhile, the glomerular filtration rate assessment provides a detailed window into how well these vital organs clean the blood.
A dangerous partnership
High blood pressure emerges as a sinister accomplice in diabetes-related kidney damage. This partnership creates a vicious cycle – diabetes makes blood pressure harder to control, while elevated pressure accelerates kidney destruction. Medical research has demonstrated that maintaining blood pressure below specific thresholds becomes crucial for protecting kidney function.
Modern medicine fights back
The medical community has developed powerful weapons in the battle against diabetic kidney damage. Specialized medications serve multiple roles, simultaneously controlling blood pressure while providing additional protection to the kidneys’ delicate filtering system. These treatments help reduce pressure within the kidneys and prevent protein loss through the urine.
Beyond medication
The path to kidney protection extends far beyond taking pills. Research reveals that daily choices dramatically impact kidney health in diabetes patients. Blood sugar control remains fundamental, as even brief periods of elevation can stress kidney tissue. A carefully planned diet, tailored to individual needs, helps maintain both blood sugar and blood pressure at safer levels.
The movement prescription
Physical activity emerges as a powerful ally in protecting kidney function. Regular movement improves blood sugar control, enhances circulation to kidney tissue, and helps maintain healthy blood pressure levels. The benefits extend beyond these direct effects, as exercise also reduces inflammation throughout the body and supports weight management.
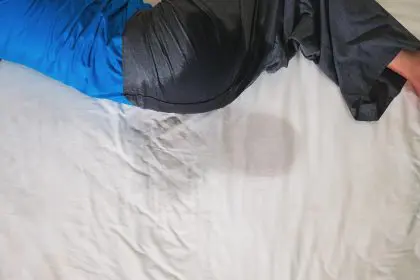
The hydration equation
While proper fluid intake supports kidney function, finding the right balance proves crucial. Individual factors such as current kidney health, blood pressure levels, and medication regimens all influence optimal hydration needs. Climate conditions and activity levels further complicate this delicate balance, making personalized guidance essential.
Medication mindfulness
The relationship between common medications and kidney health reveals another layer of complexity. Many everyday pain relievers, particularly those classified as NSAIDs, can strain already stressed kidneys. This reality necessitates careful coordination between healthcare providers and patients to ensure all medications, including over-the-counter products and supplements, work together safely.
When prevention falls short
Despite best efforts at prevention, some patients develop severe kidney damage requiring more aggressive intervention. Modern medicine offers hope through advancing transplant techniques and improved anti-rejection medications. While dialysis provides life-sustaining support, transplantation often offers better long-term outcomes and quality of life.
Vigilance as protection
Regular medical supervision stands as a cornerstone in preventing serious complications. Through consistent monitoring, healthcare providers track subtle changes in kidney function, allowing for rapid response to emerging problems. This ongoing surveillance helps guide treatment adjustments and lifestyle modifications before significant damage occurs.
Understanding personal risk
Multiple factors influence an individual’s likelihood of developing kidney problems when living with diabetes. The duration of diabetes plays a crucial role, as does family history and overall health status. Recognizing these risk factors helps healthcare providers tailor prevention strategies to each patient’s unique situation.
Hope through research
Ongoing scientific investigation continues to advance understanding of how diabetes affects kidney health. These efforts have led to new medications, improved diagnostic tools, and enhanced treatment protocols. Researchers work tirelessly to uncover genetic factors that influence kidney damage susceptibility and develop more effective prevention strategies.
Empowerment through knowledge
Understanding the connection between diabetes and kidney health empowers patients to take control of their health destiny. By recognizing early warning signs and maintaining close communication with healthcare providers, individuals can actively participate in protecting their kidney function.
A glimpse into tomorrow
While diabetes-related kidney damage presents serious challenges, modern medicine offers more hope than ever before. Early intervention, consistent monitoring, and advancing treatment options continue to improve outcomes for patients. Support systems, both medical and personal, enhance success rates in preventing and managing kidney complications.
The battle against diabetes-related kidney damage requires vigilance, commitment, and understanding. Through continued research, improved treatments, and patient education, the medical community strives to reduce the impact of this serious complication. With proper care and attention, many patients can maintain healthy kidney function despite living with diabetes, offering hope for a better future in managing this challenging condition.