The dating landscape for adults over 60 has transformed dramatically in recent years. Dating apps, active senior communities, and longer life expectancy have created new opportunities for romance – and with them, unexpected health challenges. Medical records show a steady climb in sexually transmitted disease diagnoses among older adults, yet many dismiss early warning signs as regular aging symptoms.
The truth about herpes after 60
- Herpes simplex virus affects millions of Americans, but its presentation in older adults often goes unrecognized. Rather than the obvious sores people expect, symptoms can appear as subtle skin irritation or sensitivity that many brush off as dry skin or stress-related issues. The virus can lay dormant for decades, making it particularly deceptive in the senior population.
Many older adults experience recurring symptoms without realizing the underlying cause. The burning sensation or mild discomfort might be attributed to everything from new soap to changing weather conditions, allowing the virus to spread unknowingly between partners.
Understanding HPV risks in later life
- Human papillomavirus presents a unique challenge for the older generation. While younger people often receive vaccination and education about HPV, many seniors remain unaware of their vulnerability. The virus can hibernate in the body for years before causing noticeable issues, and its connection to various cancers makes it particularly concerning.
For women over 60, regular screening remains essential, even if they’ve been in long-term relationships. The virus can activate after years of dormancy, especially when the immune system faces age-related changes.
The misunderstood symptoms of chlamydia
- Despite its reputation as a young person’s health concern, chlamydia cases among seniors continue to rise year after year. The deceptive nature of this infection lies in its ability to mirror common age-related complaints. When seniors experience mild discomfort during urination or unusual discharge, many automatically attribute these symptoms to normal aging processes or common urinary tract infections.
Medical records from senior health facilities across the country reveal a troubling pattern: chlamydia often goes undiagnosed for months or even years in older adults. This delay in treatment can lead to more severe complications, including chronic pelvic pain and inflammation that may be mistakenly attributed to arthritis or other age-related conditions.
Gonorrhea’s growing impact on senior health
- Recent health surveys indicate a significant uptick in gonorrhea diagnoses among adults over 60. The infection’s symptoms often overlap with common aging concerns: joint pain, urinary issues, and general discomfort. This similarity to everyday health changes makes it particularly challenging for both patients and healthcare providers to identify.
The rising prevalence of gonorrhea in senior communities has caught many healthcare providers off guard. Traditional screening protocols often skip STD testing for older patients, operating under outdated assumptions about senior sexuality. This oversight can allow the infection to progress, potentially leading to more serious health complications.
Why syphilis remains a hidden threat
- The resurgence of syphilis among older adults presents a particular challenge for medical professionals. Its initial symptoms – small, painless sores – often appear in places that seniors might not regularly examine or may attribute to normal skin changes. Without proper identification and treatment, the infection progresses silently, potentially causing serious damage to multiple organ systems.
Recent medical data shows an alarming trend: syphilis diagnoses among seniors frequently occur at later stages of the disease, when treatment becomes more complicated and tissue damage may already be extensive. The infection’s ability to mimic other health conditions, from arthritis to memory problems, makes it particularly dangerous for older adults.
The changing face of HIV in senior communities
- The perception of HIV as a young person’s disease has created a dangerous blind spot in senior healthcare. Adults over 60 often skip regular HIV testing, assuming their age group faces minimal risk. This misconception, combined with the virus’s ability to present like normal aging – fatigue, weight loss, cognitive changes – creates perfect conditions for delayed diagnosis.
Medical advances have transformed HIV from a death sentence into a manageable chronic condition, but early detection remains crucial. Senior communities face unique challenges in HIV prevention and treatment, including limited awareness about transmission risks and stigma surrounding testing.
The overlooked impact of trichomoniasis
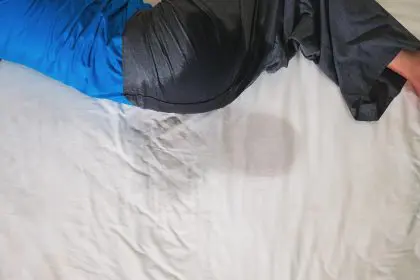
- Trichomoniasis remains one of the most frequently misdiagnosed infections among older adults. Its symptoms – irritation, discomfort, and changes in discharge – often get dismissed as vaginal dryness or normal age-related changes. This oversight allows the infection to persist, potentially increasing vulnerability to other health complications.
Recent studies indicate that trichomoniasis infections among seniors often go untreated for extended periods, creating opportunities for the parasite to affect surrounding tissues and potentially increase susceptibility to other infections.
Breaking down barriers to senior sexual health
The conversation around senior sexual health requires significant updating. Traditional healthcare approaches often overlook the sexual activity of older adults, creating gaps in preventive care and screening protocols. This oversight, combined with seniors’ own hesitation to discuss sexual health concerns, creates perfect conditions for STDs to spread undetected.
The importance of regular screening
Medical professionals emphasize that regular STD screening should continue throughout life, regardless of age or relationship status. Current guidelines recommend annual testing for sexually active adults of all ages, with more frequent screening for those with new or multiple partners.
Overcoming stigma in senior communities
The stigma surrounding STDs becomes particularly challenging in senior communities, where social connections often overlap with healthcare networks. Privacy concerns may prevent many older adults from seeking testing or treatment, even when they notice concerning symptoms.
Creating age-appropriate education
Healthcare providers increasingly recognize the need for age-appropriate sexual health education in senior communities. Traditional STD prevention messages, often targeted at younger audiences, may not resonate with older adults or address their specific concerns and circumstances.
Moving forward with awareness
The rising rates of STDs among seniors highlight the need for comprehensive healthcare approaches that recognize and respect senior sexuality. Medical professionals emphasize that maintaining sexual health represents an important aspect of overall wellness at any age.
Regular communication with healthcare providers, routine screening, and open discussions about sexual health can help seniors maintain their well-being while enjoying healthy relationships. The key lies in recognizing that sexual health remains important throughout life and deserves the same careful attention as any other aspect of senior healthcare.
Regular testing, honest conversations with healthcare providers, and staying informed about sexual health can help seniors protect themselves and their partners while maintaining active, fulfilling relationships well into their later years.