For many patients with diverse and seemingly unrelated symptoms, obtaining an accurate diagnosis can take years of specialist visits and inconclusive tests. Mast cell activation syndrome, a disorder involving immune cells gone awry, is increasingly recognized as the culprit behind many medical mysteries.
The immune sentinels that can spark chaos
The first key to understanding this complex condition involves recognizing the central role mast cells play throughout the body. These specialized immune cells serve as frontline defenders, strategically positioned in tissues that interface with the external environment including the skin, respiratory tract and digestive system.
Mast cells contain granules packed with over 200 signaling chemicals including histamine, prostaglandins, leukotrienes and cytokines. When functioning properly, they release these substances in measured response to legitimate threats like parasites or toxic substances, initiating appropriate inflammatory responses and attracting other immune cells.
In mast cell activation syndrome, these cells become hyperresponsive, releasing their chemical arsenal inappropriately in response to harmless substances or even without any identifiable trigger. This abnormal activation pattern can occur without the visible signs of increased mast cells characteristic of related conditions like mastocytosis.
Gastrointestinal mayhem often appears first
The second manifestation typically involves the digestive system. Given the high concentration of mast cells in the gastrointestinal tract, digestive symptoms frequently dominate the clinical picture. Abdominal pain, diarrhea, constipation, nausea and bloating may fluctuate in severity, often mimicking irritable bowel syndrome or inflammatory bowel disease.
Food intolerances represent another hallmark, with patients reporting reactions to historically tolerated foods, particularly those high in histamine or containing preservatives. These reactions can occur immediately or develop hours after consumption, making identification of trigger foods exceptionally challenging.
Malabsorption may develop as inflammation damages the intestinal lining, leading to nutritional deficiencies despite adequate dietary intake. Unexplained weight fluctuations and persistent fatigue often result from this combination of nutrient depletion and chronic inflammation.
Cardiovascular symptoms create diagnostic confusion
The third manifestation involves the cardiovascular system. Mast cells reside in heart tissue and throughout blood vessels, where inappropriate activation can trigger vasodilation, hypotension and tachycardia – often meeting diagnostic criteria for postural orthostatic tachycardia syndrome, a condition frequently comorbid with mast cell issues.
Patients commonly report lightheadedness upon standing, heart palpitations unrelated to exertion, and blood pressure fluctuations. These cardiovascular symptoms typically worsen after exposure to triggers and during significant mast cell activation events, creating patterns that can help alert clinicians to the underlying immune dysfunction.
Some patients experience chest pain and shortening of breath that can mimic cardiac conditions, leading to extensive cardiac workups that yield normal results despite significant symptoms. Understanding the role of mast cells helps explain this apparent disconnect between subjective experience and objective findings.
Neuropsychiatric effects extend beyond anxiety
The fourth manifestation encompasses neurological and psychiatric effects. The brain contains mast cells that, when inappropriately activated, release inflammatory mediators that affect neurotransmitter function and neural signaling. Patients commonly report brain fog, memory problems, difficulty concentrating, headaches and sleep disturbances.
Mood disturbances including anxiety and depression frequently develop, both as direct neuroinflammatory effects and as psychological responses to chronic illness. Unfortunately, these psychological symptoms may lead clinicians to attribute the entire symptom complex to anxiety, further delaying appropriate diagnosis and treatment.
Sensory sensitivity represents another neurological manifestation, with patients reporting heightened reactions to light, sound, touch and smell. These sensitivities often precede or accompany activation events, potentially serving as early warning signals of impending reactions.
Dermatological presentations vary widely
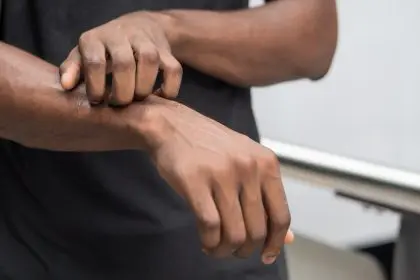
The fifth manifestation involves the skin, where mast cells reside abundantly. Flushing, hives, itching, swelling and rashes may appear, sometimes triggered by heat, pressure, sunlight or emotional stress. These dermatological symptoms often fluctuate in location and appearance, raising suspicion of allergic reactions despite negative allergy testing.
Dermatographism, where light scratching of the skin produces raised welts, occurs frequently. Some patients experience angioedema – deeper swelling that can affect the face, lips, throat or extremities – which can become alarming when respiratory structures are involved.
These skin manifestations sometimes provide the most visible evidence of mast cell dysfunction, though they may be absent in some patients whose symptoms predominate in other body systems.
Respiratory involvement mimics allergic conditions
The sixth manifestation affects the respiratory system. Nasal congestion, post-nasal drip, coughing, wheezing and shortness of breath can mimic allergic rhinitis or asthma. These symptoms often respond poorly to conventional treatments for these conditions, suggesting an alternative underlying mechanism.
Some patients develop vocal cord dysfunction or paradoxical vocal fold movement, where the vocal cords constrict inappropriately during breathing. This phenomenon can be mistaken for asthma but fails to respond to bronchodilators, creating treatment challenges until the mast cell connection is recognized.
Respiratory symptoms often worsen with exposure to airborne triggers including fragrances, smoke, pollution and volatile organic compounds, leading patients to develop lifestyle modifications to avoid these exposures.
Triggers span environmental, dietary and emotional domains
The seventh aspect involves the diverse triggers that can initiate mast cell activation events. While individual trigger profiles vary significantly, common culprits include certain foods, medications, environmental chemicals, temperature extremes, infections, hormonal fluctuations and physical or emotional stress.
This trigger diversity partly explains the elusive nature of diagnosis, as the same person might experience cardiovascular symptoms after consuming fermented foods, dermatological symptoms after heat exposure, and gastrointestinal symptoms during periods of psychological stress.
Many patients report that infections, particularly viral illnesses or tick-borne diseases, preceded their symptom onset. Research increasingly supports the concept of “mast cell priming,” where an initial severe stressor like infection or major trauma increases mast cell responsiveness to subsequent triggers.
Diagnosis requires connecting seemingly disparate symptoms
The eighth component involves the diagnostic approach. No single test definitively confirms mast cell activation syndrome. Instead, diagnosis typically involves documenting elevated mast cell mediators during symptomatic periods, ruling out other conditions, and demonstrating symptomatic improvement with medications targeting mast cell stabilization or mediator blockade.
Laboratory testing may include serum tryptase, histamine, prostaglandin D2, leukotriene E4 and 24-hour urine collections for histamine metabolites and prostaglandin metabolites. Because mediator levels fluctuate, specimens collected during asymptomatic periods often show normal results despite significant disease activity.
Clinical diagnostic criteria continue evolving as research advances, with current approaches emphasizing patterns of multi-system involvement, chronicity and response to treatment. The heterogeneous presentation and fluctuating nature of symptoms contribute to diagnostic challenges.
Management and care
Management typically involves a multi-pronged approach including trigger avoidance, H1 and H2 antihistamines, mast cell stabilizers, leukotriene modifiers and sometimes targeted nutritional interventions. For severe cases, medications like cromolyn sodium, ketotifen or low-dose naltrexone may provide additional benefit.
While still considered a relatively rare condition, many immunologists believe mast cell activation syndrome remains significantly underdiagnosed. Its protean manifestations easily masquerade as disparate conditions including chronic fatigue syndrome, fibromyalgia, irritable bowel syndrome and various autoimmune disorders.
For patients experiencing unexplained multi-system symptoms, particularly those that wax and wane or appear triggered by specific exposures, considering the mast cell connection might illuminate what previously seemed medically inexplicable. As research advances, this emerging field promises to clarify the mechanisms underlying many complex chronic illnesses and provide new therapeutic targets for intervention.