Older women experiencing increased daytime sleepiness may need to pay attention to more than just feeling tired. Revolutionary research from the University of California, San Francisco has uncovered a troubling connection between changing sleep patterns and dementia risk that could transform how we approach brain health in aging adults.
The comprehensive five-year study monitored 733 women aged 80 and above, tracking their sleep patterns and cognitive changes. Women who developed increased sleepiness over time faced double the dementia risk compared to those maintaining stable sleep patterns, adding a crucial new dimension to our understanding of dementia warning signs.
With dementia affecting over 55 million people worldwide and projected to reach 139 million by 2050, these findings arrive at a critical moment in the global effort to identify early indicators and prevention strategies for this devastating condition.
The sleep profiles that predict cognitive decline
The UCSF researchers identified three distinct sleep pattern groups among study participants, each associated with different outcomes regarding brain health.
Women with stable sleep patterns, representing nearly 44% of participants, maintained consistent sleep habits or even showed slight improvements over the study period. This group demonstrated the lowest rates of cognitive decline.
A second group, making up about 35% of participants, experienced declining nighttime sleep accompanied by increased daytime napping. These women showed moderate risk levels for cognitive issues.
Most concerning were the findings related to the third group – women experiencing increasing sleepiness both day and night, constituting about 21% of participants. This group faced significantly higher dementia risk, suggesting their changing sleep needs might reflect underlying neurological changes.
By the end of the five-year follow-up period, nearly 13% of all participants had developed dementia, while over 22% had progressed to mild cognitive impairment, often considered a precursor to dementia.
The chicken-or-egg question: Does poor sleep cause dementia or vice versa?
The relationship between sleep disturbances and dementia appears increasingly complex, according to experts analyzing the groundbreaking research.
Dr. Ben Dunkley, a cognitive neuroscientist not involved in the study, describes the connection as bidirectional, explaining that increased sleepiness may signal early neurodegenerative changes while dementia-related damage can simultaneously disrupt brain regions responsible for regulating sleep.
This creates what researchers call a “feedback loop” where each condition potentially worsens the other. Sleep disruption may accelerate neurological damage, while progressing brain changes further destabilize sleep patterns.
The study’s findings align with previous research suggesting sleep disturbances often appear years before other recognizable dementia symptoms, potentially offering a valuable early warning sign for healthcare providers and families.
Beyond sleepiness: Other dementia risk factors to know
While the sleep-dementia connection represents an important breakthrough, experts emphasize that multiple factors influence cognitive health as we age.
The Centers for Disease Control and Prevention identifies several modifiable risk factors for dementia beyond sleep issues. Physical inactivity remains a significant concern, with sedentary lifestyles linked to faster cognitive decline across numerous studies.
Unmanaged chronic conditions like diabetes and hypertension can damage blood vessels throughout the body, including those supplying the brain, creating conditions favorable for dementia development.
Hearing loss, often overlooked in discussions about brain health, has emerged as a surprisingly significant risk factor. Experts theorize that the increased cognitive effort required to process sounds with hearing impairment may divert resources from other brain functions, accelerating decline.
Lifestyle choices including tobacco and alcohol use continue to show strong associations with increased dementia risk, with smokers facing up to 50% higher rates according to some studies.
Protecting brain health through better sleep habits
The UCSF study suggests maintaining healthy sleep patterns could prove crucial for preserving cognitive function, especially for women in their later years.
Sleep experts recommend establishing consistent sleep schedules, going to bed and waking at approximately the same times each day to regulate the body’s internal clock. This practice helps optimize sleep quality and potentially supports brain health.
Creating an environment conducive to restful sleep represents another important step. This includes maintaining comfortable room temperatures, minimizing light and noise disturbances, and limiting screen time before bed.
Physical activity during the day has consistently shown benefits for nighttime sleep quality. Even light exercise like walking can help regulate sleep cycles and may offer dual protection against dementia through both sleep improvement and direct brain benefits.
Monitoring and addressing sleep disorders becomes increasingly important with age. Conditions like sleep apnea, which causes breathing interruptions during sleep, have been linked to higher dementia risk when left untreated.
When changing sleep patterns warrant medical attention
While occasional sleepiness represents a normal part of life, certain changes merit discussion with healthcare providers, particularly for older adults.
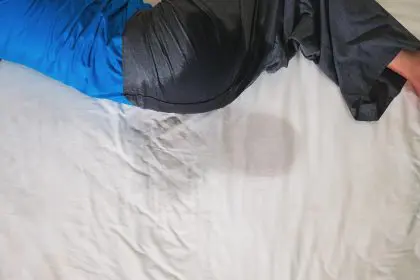
Needing significantly more sleep than usual or experiencing excessive daytime drowsiness despite adequate nighttime rest could indicate underlying issues requiring attention. These changes often develop gradually, making them easy to dismiss or normalize.
Frequent sleep interruptions or difficulty maintaining sleep throughout the night may also signal problems. Many older adults experience these issues but mistakenly consider them inevitable consequences of aging rather than potentially treatable conditions.
Sleep specialists now have access to improved diagnostic tools, including sophisticated wearable monitors that track sleep patterns over extended periods. These devices can reveal disruptions that might otherwise go unnoticed during brief medical appointments.
The future of dementia prevention
As research continues unveiling connections between sleep and brain health, scientists express cautious optimism about developing more effective prevention strategies.
Dr. Steve Allder, a consultant neurologist commenting on the study findings, notes that understanding sleep’s role in cognitive health opens new possibilities for intervention. “We now recognize that addressing sleep disturbances may represent a modifiable risk factor for dementia, similar to managing blood pressure or increasing physical activity,” he explains.
The UCSF research team plans follow-up studies to determine whether interventions targeting sleep can measurably reduce dementia rates. These studies may include testing sleep medications, cognitive behavioral therapy for insomnia, and technology-assisted sleep improvement programs.
Some research centers have begun investigating whether altering specific sleep stages might protect brain function. Deep sleep appears particularly important for clearing potentially harmful proteins from the brain, including those associated with Alzheimer’s disease.
Public health experts suggest the findings should influence how we approach aging and brain health at both individual and community levels. Raising awareness about sleep’s critical role in cognitive function could empower more people to prioritize rest as an essential health practice rather than a luxury.
For women in particular, these findings highlight the importance of discussing sleep changes with healthcare providers rather than dismissing them as inevitable aspects of aging. Recognizing and addressing sleep disturbances early might ultimately provide a valuable opportunity to intervene before cognitive decline advances.
As our understanding of the sleep-dementia connection deepens, it increasingly appears that quality rest represents not merely a comfort but a fundamental requirement for brain health throughout life—and particularly in our later years.