The beauty and wellness industry continues introducing innovative products promising simpler solutions to everyday concerns, with oral sunscreens representing one of the most intriguing recent developments. These supplements claim to protect skin from harmful ultraviolet rays through ingested ingredients rather than topical application, appealing to those seeking convenience over traditional lotions and sprays. But the science behind these products reveals a more complicated reality than their marketing suggests.
The science behind ingestible sun protection
Oral sunscreens, more accurately described as photoprotective supplements, contain various compounds theorized to enhance skin’s natural defense mechanisms against solar damage. 1) The primary ingredient in many formulations, Polypodium leucotomos extract (PLE), comes from a tropical fern native to Central and South America with centuries of traditional medicinal use for skin conditions.
This extract contains antioxidant compounds that may help neutralize free radicals generated during sun exposure. Laboratory studies show these compounds might reduce DNA damage, inflammation, and oxidative stress resulting from ultraviolet radiation. The appeal comes from addressing sun damage at the cellular level rather than simply creating a physical barrier as topical sunscreens do.
Other common ingredients in these formulations include nicotinamide (vitamin B3), which supports DNA repair mechanisms potentially damaged by UV exposure. Astaxanthin, a carotenoid derived from microalgae, provides powerful antioxidant properties that may help mitigate oxidative stress. Lycopene, the compound that gives tomatoes their red color, has shown potential in supporting skin‘s resilience against UV damage in preliminary research.
Despite the theoretical benefits of these ingredients, the challenge lies in determining whether ingested compounds can adequately concentrate in skin tissue to provide meaningful protection against the immediate and cumulative effects of sun exposure.
Limited evidence raises concerns
The research supporting oral sunscreen efficacy remains significantly more limited than studies validating traditional sunscreen. 2) While several small clinical trials show promising results for specific ingredients, particularly Polypodium leucotomos extract, these studies typically involve small participant groups and often measure secondary markers rather than direct sun protection.
One frequently cited 2015 study found participants taking PLE experienced less sunburn when exposed to controlled UV radiation compared to those taking a placebo. However, the actual level of protection fell far below what quality topical sunscreens provide. The study showed modest protection equivalent to approximately SPF 3-5, considerably lower than the SPF 30 minimum recommended for adequate sun protection.
Research gaps become particularly concerning when considering the unpredictable nature of how individual bodies process supplements. Factors including metabolism, existing nutrition status, and medication interactions can significantly influence how effectively these compounds concentrate in skin tissue. This variability makes standardizing dosage recommendations and protection claims exceptionally difficult.
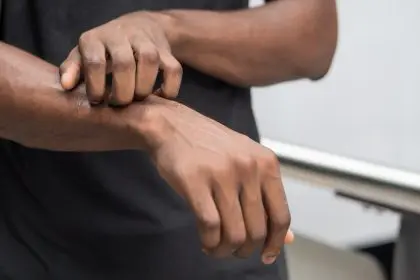
The limited scope of existing research also means we lack comprehensive understanding of these supplements’ effectiveness across diverse skin types, conditions, and demographics. With melanoma rates continuing to rise nationwide, this uncertainty poses legitimate public health concerns.
False security creates dangerous scenario
Perhaps the greatest risk associated with oral sunscreens involves the false sense of security they potentially create. 3) Marketing language sometimes suggests these products provide complete protection, leading some consumers to believe they can forgo traditional sunscreen application altogether — a dangerous misconception that could increase skin cancer risk.
This misunderstanding proves particularly problematic considering the modest protection levels these supplements might provide at best. Even if the ingredients work exactly as theorized, the protection level falls significantly below recommended standards for preventing skin damage. Most dermatology experts agree that if used at all, these supplements should only complement comprehensive sun protection strategies, never replace proven methods.
The supplement classification itself contributes to consumer confusion. Unlike topical sunscreens regulated as over-the-counter drugs with standardized testing requirements for SPF claims, oral sunscreens fall under dietary supplement regulations with significantly less oversight. This classification means manufacturers cannot legally make specific SPF claims, though marketing materials sometimes imply protection levels through careful wording.
The lack of standardized testing protocols for these products means consumers have no reliable way to compare protection between different oral sunscreen formulations or understand how they might complement traditional protection methods.
Regulatory concerns remain unaddressed
The regulatory framework governing these products raises additional questions about their reliability and safety. 4) As dietary supplements rather than drugs, oral sunscreens undergo minimal pre-market testing requirements compared to topical sunscreens. The Food and Drug Administration does not evaluate these products for safety or efficacy before they reach consumers.
This limited oversight means manufacturing quality, ingredient purity, and dosage accuracy depend largely on individual companies’ internal standards rather than universal requirements. Independent testing has sometimes revealed significant discrepancies between labeled ingredients and actual contents in various supplement categories, raising questions about consistency across the industry.
Interactions with medications present another concern lacking sufficient research. Polypodium leucotomos has immunomodulating properties that could potentially interfere with immunosuppressive medications. Other common ingredients like astaxanthin and lycopene may interact with blood thinners or hormone medications. Without thorough clinical evaluation, these potential interactions remain poorly understood.
Pregnancy and breastfeeding safety represents another area with insufficient data. Many oral sunscreen manufacturers recommend against use during pregnancy due to this research gap, though this caution often appears in fine print rather than prominent warnings.
Proper sun protection requires comprehensive approach
Established dermatology guidelines continue emphasizing that effective sun protection requires multiple strategies working together. 5) Regardless of whether someone chooses to incorporate photoprotective supplements, traditional methods remain essential for preventing skin damage, premature aging, and cancer risk.
Broad-spectrum topical sunscreen with minimum SPF 30, reapplied every two hours during sun exposure, provides the foundation of effective protection. Physical barriers including wide-brimmed hats, sunglasses with UV protection, and UPF-rated clothing offer additional defense against harmful rays. Seeking shade, particularly during peak UV hours between 10 a.m. and 2 p.m., further reduces exposure risk.
For those considering adding oral supplements to this regimen, understanding their limitations proves crucial. Rather than viewing them as standalone protection, they might better serve as supplementary support to comprehensive sun safety habits. Individuals with specific concerns like photosensitivity disorders or extremely high skin cancer risk might benefit most from this additive approach after consulting healthcare providers.
The timing of supplementation also influences potential effectiveness. Most research suggests these products work best when taken consistently for at least 7-14 days before significant sun exposure rather than as last-minute protection. This requirement further emphasizes they cannot replace immediate protection methods like traditional sunscreen.
Who might benefit from supplementary approach
Despite limitations, certain populations might find value in adding photoprotective supplements to comprehensive sun protection regimens. 6) Individuals with histories of skin cancer or precancerous lesions sometimes seek every available protective measure, making supplements a potential addition to their existing routines after medical consultation.
Those with photosensitive conditions like polymorphous light eruption or certain autoimmune disorders affecting sun tolerance may experience modest benefits from the anti-inflammatory properties these supplements often provide. The reduced inflammation might help manage symptoms, though direct sun protection still requires traditional methods.
Athletes and outdoor workers with extensive sun exposure despite using traditional protection might consider these supplements as additional support rather than replacement protection. The potential cellular-level effects could theoretically complement external barriers, though comprehensive sun safety practices remain essential.
Individuals with difficulty applying traditional sunscreen due to mobility issues or certain skin conditions sometimes explore oral options. However, physical barriers like protective clothing typically provide more reliable alternatives when topical application proves challenging.
The future of sun protection research
Ongoing research may eventually clarify the role these supplements could play in comprehensive sun protection strategies. Several larger clinical trials currently underway aim to better quantify protection levels, standardize effective dosages, and clarify which populations might benefit most from these products.
Technological advances in measuring cellular damage from UV exposure now allow more precise evaluation of protection mechanisms. These methods move beyond simply measuring sunburn to assess deeper cellular impacts, potentially providing more meaningful data about supplement effectiveness.
Combination formulations incorporating multiple photoprotective compounds are also undergoing evaluation. These products aim to provide synergistic benefits addressing different aspects of UV damage simultaneously. While promising in theory, these complex formulations require thorough evaluation for both effectiveness and safety.
Despite these research advances, most dermatology experts maintain skepticism about whether oral products will ever match the protection level of quality topical sunscreens. The fundamental challenge involves delivering sufficient active compounds specifically to skin tissue where protection is needed most.
Making informed decisions about sun protection
For consumers navigating conflicting claims about oral sunscreens, focusing on established facts rather than marketing promises offers the clearest guidance. No oral supplement currently on the market provides adequate standalone sun protection according to established dermatology standards. Traditional sunscreen, protective clothing, and sun avoidance remain essential regardless of supplement use.
Those still interested in exploring oral products should approach them as potential supplements to proven methods rather than replacements. Consulting healthcare providers before starting any new supplement regimen allows for personalized guidance based on individual health conditions, medication use, and skin cancer risk factors.
Reading product labels critically helps identify questionable marketing claims. Terms like “sunscreen pill” or specific SPF equivalency claims should raise red flags, as these statements exceed what research currently supports and what regulations allow.
The appeal of simplified sun protection through a daily pill remains understandable in our convenience-focused culture. However, the science simply hasn’t caught up with this appealing concept. Until more robust evidence emerges, comprehensive sun protection still requires the multi-faceted approach dermatology experts have recommended for decades.
As research continues advancing our understanding of these products, the most prudent approach balances openness to innovation with healthy skepticism about claims exceeding current evidence. The skin health consequences of inadequate sun protection prove too significant to trust unproven methods over established protection strategies that demonstrably reduce cancer risk and prevent premature aging.