This troublesome respiratory condition goes beyond typical allergy symptoms and requires specific treatment approaches
When allergies attack your airways
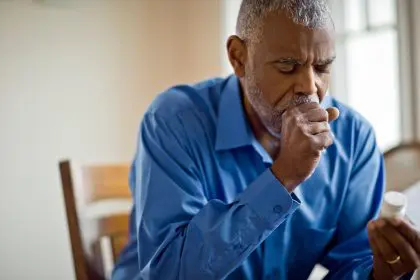
For millions of Americans, seasonal allergies bring the familiar annoyance of sneezing, itchy eyes, and congestion. But for some, these allergic reactions extend deeper into the respiratory system, triggering a more serious condition known as allergic bronchitis. This often-overlooked respiratory ailment can significantly impact your quality of life, causing persistent coughing and breathing difficulties that over-the-counter allergy medications fail to resolve.
Unlike typical allergies that primarily affect the upper respiratory tract, allergic bronchitis specifically inflames the bronchial tubes – the vital airways that carry oxygen to your lungs. This inflammation narrows these passages, making breathing difficult and triggering a persistent cough that can last for months. Understanding this condition is crucial for proper treatment, especially since its symptoms can be mistaken for other respiratory problems.
The surprising link between allergies and bronchitis
Most people recognize allergies as immune system overreactions to otherwise harmless substances like pollen, pet dander, or dust mites. When exposed to these triggers, your body releases chemicals like histamine that cause inflammation in your nose, sinuses, and throat – resulting in the classic allergy symptoms we all know.
However, in some individuals, this inflammatory response doesn’t stop at the upper airways. The same allergens can penetrate deeper, irritating the sensitive lining of the bronchial tubes. Over time, especially with repeated exposure, this irritation leads to allergic bronchitis – a condition that combines the hallmarks of both allergies and bronchial inflammation.
This connection explains why many people develop bronchitis symptoms during allergy season or after prolonged exposure to indoor allergens. While not everyone with allergies will develop bronchitis, those with asthma or other respiratory conditions face a higher risk of this complication, as do those with compromised immune systems or frequent respiratory infections.
The 7 telltale symptoms that differentiate allergic bronchitis
Distinguishing allergic bronchitis from standard allergies or even a common cold requires knowing these key symptoms:
A persistent wet cough that produces mucus stands as the most prominent symptom of allergic bronchitis. Unlike the dry, tickling cough of typical allergies, this cough brings up phlegm and often worsens at night or early morning. This mucus production happens as your inflamed airways produce extra secretions to try to flush out perceived irritants.
The characteristic wheezing sound when breathing – a high-pitched whistling or squeaking noise – occurs when air forces its way through narrowed bronchial passages. This sound typically becomes more pronounced during physical exertion or when lying down at night.
Many patients report a constant tightness or pressure in their chest, similar to the feeling of someone sitting on their chest. This uncomfortable sensation results from the bronchial inflammation and muscle constriction around the airways.
Beyond the typical fatigue that allergies might cause, allergic bronchitis often brings a deeper exhaustion. The combination of poor sleep due to coughing, reduced oxygen intake, and the body’s energy expenditure fighting inflammation leaves many patients feeling profoundly tired.
While regular allergies might make exercise uncomfortable, allergic bronchitis can make even moderate activity feel impossible. Many patients find themselves struggling to catch their breath after climbing stairs or walking short distances, as the narrowed airways limit oxygen flow during increased physical demands.
Unlike seasonal allergies that come and go, allergic bronchitis symptoms often persist for extended periods – sometimes lasting three months or longer. When the condition becomes chronic, these symptoms may return yearly for multiple consecutive years.
Beyond the bronchitis-specific symptoms, patients typically experience traditional allergy signs simultaneously – including sneezing, itchy or watery eyes, runny nose, and sometimes skin rashes. These symptoms often intensify shortly before the bronchitis symptoms flare up.
What triggers this troublesome condition
Environmental factors play a significant role in both triggering and exacerbating allergic bronchitis. Understanding these common triggers can help you take proactive steps to avoid them:
Tobacco smoke ranks among the most damaging irritants for those with allergic bronchitis. Whether you’re smoking yourself or exposed to secondhand smoke, the chemicals in tobacco smoke directly irritate the bronchial lining and worsen inflammation. Even third-hand smoke – the residue that clings to clothes and furniture – can trigger symptoms in highly sensitive individuals.
Urban air pollution, including vehicle exhaust, industrial emissions, and smog, contains particulate matter and chemicals that can penetrate deep into the airways. During high pollution days, those with allergic bronchitis often experience significant symptom flare-ups, making air quality monitoring an essential part of managing this condition.
Workplace exposures to chemical fumes, dust, or other airborne irritants represent a major trigger for many patients. Occupations involving cleaning products, paint, construction materials, or manufacturing processes carry particular risks. Even office environments can harbor triggers like printer toner particles, perfumes, or cleaning solutions.
Common household allergens, including dust mites, pet dander, and mold spores, frequently trigger allergic bronchitis symptoms. These microscopic irritants easily become airborne and penetrate deep into the respiratory system, making home environments potential hotspots for symptom flares.
In addition to these primary triggers, cold air, respiratory infections, and even stress can worsen allergic bronchitis symptoms in many patients. The condition often involves a complex interplay of multiple factors, making comprehensive management approaches necessary.
The treatment approaches that bring relief
Effectively managing allergic bronchitis requires a multi-faceted approach tailored to your specific triggers and symptoms. While the condition can be challenging to control completely, these treatment strategies can significantly improve quality of life:
Bronchodilator medications work by relaxing the muscles around the airways, opening them wider to improve airflow. These medications, typically delivered through inhalers, provide relatively quick relief when breathing becomes difficult. For allergic bronchitis, healthcare providers often prescribe both short-acting bronchodilators for immediate symptom relief and long-acting versions for ongoing management.
Anti-inflammatory treatments directly target the underlying inflammation in the bronchial tubes. Inhaled corticosteroids represent the most common option, reducing swelling and mucus production in the airways over time. Unlike bronchodilators, these medications don’t provide immediate relief but instead work gradually to decrease the frequency and severity of symptoms when used consistently.
For patients whose symptoms include significant mucus production, mucolytic medications help thin and loosen the secretions, making them easier to cough up and clear from the airways. These medications come in both prescription and over-the-counter formulations.
Allergy control forms a crucial component of allergic bronchitis management. Antihistamines and nasal corticosteroids help control upper respiratory allergy symptoms, while allergen immunotherapy (allergy shots) can reduce overall sensitivity to specific triggers over time.
For those with severe symptoms or frequent flare-ups, pulmonary rehabilitation programs offer comprehensive support. These structured programs combine exercise training, breathing techniques, nutritional counseling, and education to improve lung function and overall quality of life.
Home strategies that protect your lungs
Beyond medical treatments, implementing these practical home strategies can significantly reduce exposure to triggers and minimize symptoms:
Investing in high-quality air purifiers with HEPA filtration can capture most airborne allergens and irritants. Placing these units in bedrooms and frequently used living spaces creates “clean air zones” where your respiratory system can get a break from constant irritation.
Regular damp dusting and vacuuming with a HEPA-filtered vacuum helps control dust mites and other indoor allergens. Washing bedding weekly in hot water, using allergen-proof mattress and pillow covers, and reducing household clutter all contribute to lower allergen levels.
Controlling indoor humidity between 40-50% helps prevent mold growth while also keeping dust mites in check. In humid climates, dehumidifiers play an essential role in maintaining this optimal range, particularly in basements and bathrooms where moisture tends to accumulate.
Smoking cessation represents perhaps the single most important step for smokers with allergic bronchitis. The relationship between smoking and bronchial inflammation is so direct that continued smoking essentially counteracts all other treatment efforts. Support programs, medications, and counseling can help overcome this addiction.
Establishing an exercise routine appropriate for your current lung function helps strengthen respiratory muscles and improve overall lung capacity. Starting with gentle activities like walking or swimming and gradually increasing intensity offers the best approach for most patients.
When to seek urgent medical attention
While allergic bronchitis typically doesn’t represent an immediate medical emergency, certain warning signs indicate the need for prompt medical evaluation:
If you experience sudden, severe difficulty breathing or feel like you can’t get enough air, seek emergency care immediately. This could indicate a severe bronchospasm or another serious respiratory complication requiring immediate intervention.
A fever above 101°F (38.3°C) alongside bronchitis symptoms suggests a possible infection rather than just allergic inflammation. Bacterial infections can develop on top of allergic bronchitis and may require antibiotic treatment.
If your mucus changes from clear or white to yellow, green, or rust-colored, this often indicates a bacterial infection has developed. Similarly, bloody mucus warrants immediate medical attention to rule out more serious conditions.
Symptoms that progressively worsen despite treatment, or new symptoms like chest pain that doesn’t seem related to coughing, require prompt medical evaluation. These changes might indicate the development of complications or possibly a different underlying condition.
For those with known asthma alongside allergic bronchitis, using rescue inhalers more frequently than prescribed or finding them less effective than usual represents a warning sign that requires medical attention. This pattern often indicates worsening airway inflammation that needs treatment adjustment.
The long-term outlook for your breathing health
With proper management, most people with allergic bronchitis can expect significant symptom improvement and a good quality of life. However, understanding the long-term implications helps set realistic expectations:
For some individuals, allergic bronchitis represents a temporary condition that resolves completely with proper treatment and allergen avoidance. Others may experience recurrent episodes, particularly during allergy seasons or after specific exposures.
When symptoms persist for more than three months yearly for at least two consecutive years, the condition may be classified as chronic bronchitis – a form of chronic obstructive pulmonary disease (COPD). Early and aggressive management helps prevent this progression in many cases.
Over time, repeated cycles of bronchial inflammation can lead to permanent changes in airway structure – a process called “airway remodeling.” This underscores the importance of consistent treatment, even during symptom-free periods, to protect long-term lung function.
Regular follow-up with healthcare providers allows for treatment adjustments as needed and monitoring of lung function over time. Pulmonary function tests provide objective measurements of how well your lungs work and help guide treatment decisions.
With the right combination of medical treatment, environmental modifications, and self-care strategies, most people with allergic bronchitis learn to effectively manage their condition and maintain an active, fulfilling lifestyle despite this respiratory challenge.