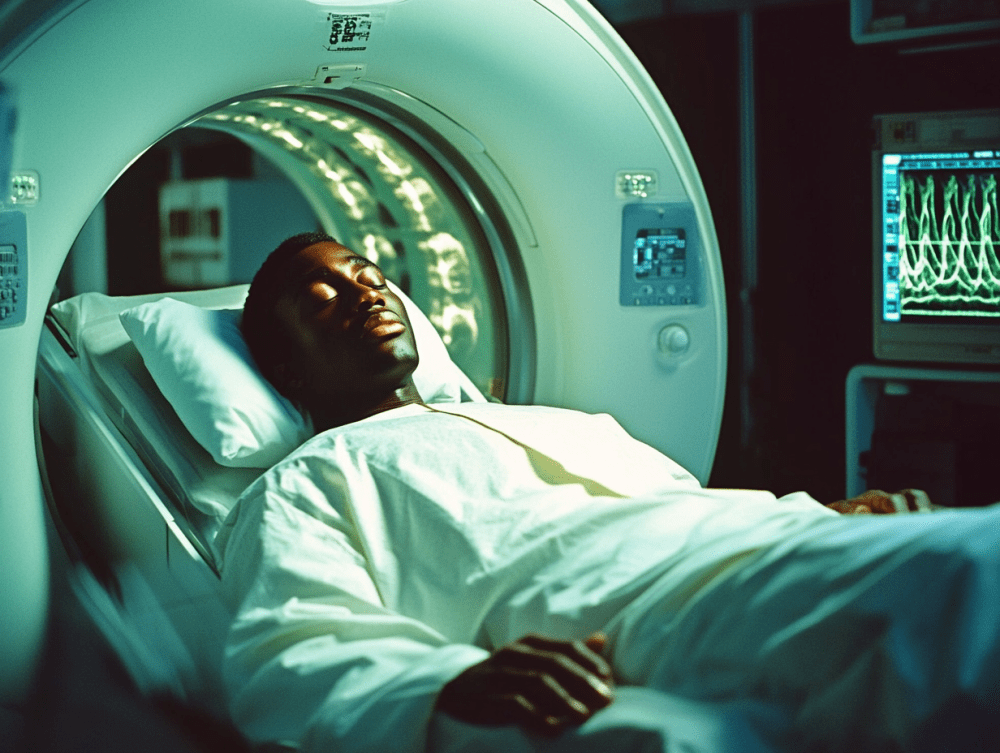
While these advanced imaging tools save lives by detecting injuries and illness, mounting evidence suggests they may come with long-term consequences that patients need to understand before agreeing to scans.
Computed tomography (CT) scans have revolutionized modern medicine, allowing healthcare providers to see inside the human body with remarkable clarity without invasive procedures. These diagnostic marvels help detect everything from brain injuries after accidents to tiny tumors that might otherwise remain hidden until symptoms appear.
Yet recent research has cast a shadow over this essential medical tool. A new study published in JAMA Internal Medicine has found that CT scans may be responsible for approximately 5% of annual cancer diagnoses in the United States. This startling statistic has raised important questions about the balance between immediate diagnostic benefits and potential long-term health risks.
The alarming rise in CT scan usage nationwide
CT scanning technology has become increasingly common in American healthcare facilities, with usage surging approximately 30% since 2007. Several factors drive this growth, including aging population demographics, technological advancements making scans faster and more detailed, and evolving medical practices that increasingly rely on imaging.
In 2023 alone, medical facilities performed roughly 93 million CT scans on 61.5 million Americans. This staggering number represents nearly one-fifth of the entire U.S. population receiving at least one scan within a single year. Many patients undergo multiple scans, particularly those with chronic conditions or those receiving cancer treatment.
The rise in scanning frequency stems partly from medical necessity, but healthcare experts note concerning trends in unnecessary scanning. Time pressures on physicians can make ordering a scan seem more efficient than conducting lengthy diagnostic interviews. Additionally, patient expectations sometimes drive scan requests even when limited clinical evidence suggests they would provide useful information.
This widespread adoption of CT technology means millions more Americans face radiation exposure each year, making the potential cancer link a significant public health concern worthy of serious attention.
How ionizing radiation damages cellular DNA
CT scans employ ionizing radiation to create detailed cross-sectional images of internal body structures. While medical professionals have always recognized that this radiation carries risks, recent research has clarified the biological mechanisms through which CT scans potentially contribute to cancer development.
The ionizing radiation from CT scans can damage DNA within cells, creating breaks in the genetic material essential to proper cellular function. While the human body has sophisticated repair mechanisms that can fix most DNA damage, these mechanisms aren’t perfect. Some damage persists, potentially leading to mutations that can eventually trigger cancerous cell growth.
The radiation doses from medical imaging differ significantly from those experienced in environmental exposure scenarios. A single chest CT scan delivers approximately 70 times the radiation of a standard chest X-ray. More concerning, some complex CT procedures may expose patients to radiation levels comparable to those experienced by some survivors at the periphery of the Hiroshima atomic bomb blast.
Different tissues demonstrate varying sensitivity to radiation damage. Breast tissue, thyroid glands, and bone marrow prove particularly vulnerable, especially in younger patients whose rapidly dividing cells face greater risk from radiation-induced DNA damage.
Future cancer cases linked to current scanning practices
The recent JAMA Internal Medicine study employed mathematical modeling based on patient demographics and radiation exposure data to estimate potential future implications of current CT usage patterns. Researchers projected that CT scans performed in 2023 alone could eventually lead to approximately 103,000 future cancer cases.
These projected cancers would affect various organs, with lung, colon, and breast cancers representing the most common types attributed to CT radiation exposure. The onset of these cancers typically occurs years or even decades after radiation exposure, making the connection difficult for patients and healthcare providers to recognize.
Important caveats accompany these projections. The estimates derive from mathematical models rather than direct observation of patient outcomes. These models incorporate assumptions about how radiation affects human cells based on historical radiation exposure events and laboratory studies. While representing the best available science, uncertainty remains about precise cancer risk levels from medical imaging.
Despite these limitations, medical authorities consider the fundamental connection between radiation exposure and cancer risk well-established. The significant question isn’t whether CT scans cause some cancers, but rather how many cases result from medical imaging and how to minimize this number without sacrificing essential diagnostic capabilities.
Children face heightened vulnerability to scanning risks
Research indicates particularly concerning risks for pediatric patients. Infants scanned before their first birthdays may face up to ten times higher cancer risk compared to adults receiving identical scans. This heightened vulnerability stems from several factors unique to younger patients.
Children’s rapidly developing tissues contain more dividing cells susceptible to radiation damage. Their smaller bodies mean radiation passes through less tissue, potentially delivering higher effective doses to sensitive organs. Additionally, children have longer remaining lifespans during which radiation-damaged cells can ultimately develop into cancers.
Despite these elevated risks, adults undergo significantly more CT scans annually, accounting for the majority of estimated future cancer cases. The total cancer burden remains primarily an adult health concern simply due to the vastly larger number of scans performed on adult patients.
Medical imaging specialists have developed pediatric-specific protocols that reduce radiation exposure while maintaining diagnostic quality. Parents should ask specifically about these child-appropriate techniques when their children require imaging studies, particularly for non-emergency situations where time exists to ensure proper protocols.
Balancing necessary diagnosis against potential harm
The concerning statistics about cancer risk must be considered alongside the life-saving benefits CT scans provide. In emergency situations, these scans rapidly identify life-threatening conditions like brain hemorrhages, aortic dissections, or internal injuries following accidents. In these scenarios, the immediate benefits clearly outweigh potential future risks.
For less urgent conditions, patients and healthcare providers should engage in more nuanced discussions about imaging choices. Alternative imaging methods like magnetic resonance imaging (MRI) or ultrasound may provide similar diagnostic information without radiation exposure. While these alternatives may cost more or take longer to perform, they eliminate radiation-related cancer risks entirely.
When CT scans prove medically necessary, technological advancements now allow for significant radiation dose reductions while maintaining diagnostic image quality. Patients should inquire specifically about whether facilities use dose-reduction technologies and protocols, particularly for scans involving sensitive areas like the chest or abdomen.
Medical experts suggest patients ask several key questions before agreeing to CT scans, including whether the scan will influence treatment decisions, what information it will provide that cannot be obtained through other means, and whether radiation-free alternatives might suffice. For follow-up scans monitoring known conditions, patients might inquire about lengthening intervals between imaging sessions when clinically appropriate.
Advocating for appropriate imaging practices
Patients can take proactive steps to reduce unnecessary radiation exposure while still receiving appropriate medical care. The simplest approach involves avoiding truly unnecessary scans, particularly those unlikely to change treatment decisions or provide clinically useful information.
When scans prove necessary, patients should inquire about facilities’ radiation dose protocols. Substantial variation exists between imaging centers, with some routinely employing significantly higher radiation levels than required for adequate diagnostic quality. Patients might specifically ask whether facilities use “dose optimization” techniques that minimize radiation while maintaining image quality.
Medical imaging records should be carefully maintained and shared between healthcare providers to prevent duplicate scans when patients change medical facilities. Electronic medical record systems increasingly include radiation dose tracking features, allowing providers to monitor cumulative exposure over time, though these systems remain inconsistently implemented.
Professional medical organizations have developed appropriateness criteria to guide imaging decisions. Patients might ask whether recommended scans align with these evidence-based guidelines, particularly for situations where the clinical value of imaging remains uncertain or controversial.
Emerging technologies that may reduce future risks
The medical imaging field continues advancing rapidly, with several promising developments potentially reducing cancer risks associated with CT scanning. These innovations focus on both reducing radiation doses and developing alternative imaging approaches that eliminate radiation entirely.
Artificial intelligence applications now enhance images captured at lower radiation doses, maintaining diagnostic quality while reducing exposure. These machine learning algorithms effectively “clean up” images that would previously have appeared too grainy or unclear for diagnosis, allowing for substantial radiation reduction.
Photon-counting CT represents a significant technological leap, using fundamentally different detection methods that capture more information from each radiation particle. These next-generation scanners potentially reduce radiation requirements by 40-70% while providing superior image quality and additional diagnostic information.
Advanced MRI techniques continue expanding the range of conditions diagnosable without radiation. While traditionally slower and more expensive than CT, newer MRI protocols provide faster scanning times and enhanced capabilities for evaluating conditions previously requiring CT imaging.
These technological advancements, combined with growing awareness about radiation risks, suggest that future medical imaging may provide even greater diagnostic value with substantially reduced cancer risk, continuing the medical tradition of balancing benefits against potential harms.
Making informed decisions about medical imaging
The relationship between CT scans and cancer risk highlights the importance of informed medical decision-making. While these scans represent remarkable diagnostic tools that save countless lives, their usage requires thoughtful consideration of both immediate benefits and potential long-term consequences.
Patients should view healthcare providers as partners in making appropriate imaging decisions. By asking questions about scan necessity, potential alternatives, and radiation dose minimization, patients can actively participate in balancing diagnostic needs against radiation exposure concerns.
For patients requiring multiple scans over time, discussing cumulative radiation exposure with healthcare providers becomes particularly important. Radiation effects accumulate throughout life, with each exposure incrementally increasing cancer risk. Tracking total exposure helps inform decisions about whether additional scans justify their potential risks.
The medical community continues refining guidelines about appropriate imaging usage, with increasing emphasis on avoiding unnecessary radiation exposure. These evolving standards aim to preserve the tremendous diagnostic benefits CT scans provide while minimizing the number of future cancers attributable to medical imaging.
Ultimately, CT scans exemplify modern medicine’s complex risk-benefit calculations. Their ability to non-invasively visualize internal structures has transformed patient care, while their radiation-related risks remind us that even the most valuable medical tools require judicious application guided by scientific evidence, clinical expertise, and patient preferences.