Psoriatic arthritis combines painful joint inflammation with skin symptoms, creating unique challenges for those affected. Understanding these warning signs can lead to earlier diagnosis and better long-term outcomes.
Psoriatic arthritis (PsA) presents a complex challenge for millions of people worldwide. This chronic autoimmune condition merges the joint pain and inflammation of arthritis with the skin manifestations of psoriasis, creating a dual-symptom disease that requires specialized care.
Most people who develop PsA already have psoriasis, though the joint symptoms can occasionally appear first. This condition occurs when the immune system mistakenly attacks healthy cells and tissue, causing inflammation in joints and overproduction of skin cells. The result is both painful, swollen joints and patches of red, scaly skin that can significantly impact quality of life.
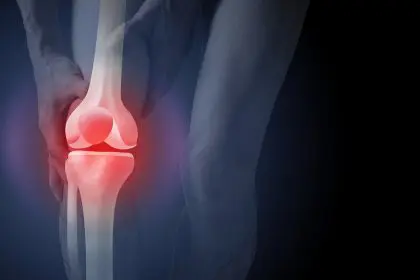
Joint pain and inflammation patterns
The hallmark of psoriatic arthritis is joint pain that often follows distinctive patterns. For many, the discomfort begins in smaller joints, particularly the fingers and toes, creating a sausage-like swelling called dactylitis. This distinctive feature helps differentiate PsA from other forms of arthritis.
The pain typically feels worse in the morning or after periods of inactivity, with stiffness that gradually improves with movement. Unlike some other forms of arthritis, PsA can affect joints asymmetrically, meaning it might affect different joints on opposite sides of the body.
For approximately 30 percent of patients, the spine becomes involved in what’s known as psoriatic spondylitis. This manifestation causes inflammation in the spinal joints and the places where tendons and ligaments attach to bones, leading to persistent back pain that improves with activity but worsens with rest.
The inflammatory nature of PsA means that affected joints often appear red and feel warm to the touch. This active inflammation distinguishes it from wear-and-tear arthritis conditions and signals the underlying immune system malfunction driving the disease.
Skin manifestations and their connection to joint symptoms
Most people with psoriatic arthritis experience skin symptoms before joint pain develops. The characteristic psoriasis plaques appear as raised, red patches covered with silvery-white scales, most commonly on the elbows, knees, scalp, and around the ears.
These plaques develop because the immune system triggers skin cells to multiply much faster than normal – completing their life cycle in days rather than weeks. The excess skin cells build up into the visible patches that can crack, itch, and sometimes bleed.
The severity of skin symptoms doesn’t necessarily correlate with joint inflammation. Some individuals with extensive psoriasis experience minimal joint problems, while others with limited skin involvement suffer significant arthritis symptoms.
The genetic factors that predispose someone to psoriasis also increase their risk of developing psoriatic arthritis. For this reason, anyone with psoriasis should pay close attention to new joint pain or stiffness and report these symptoms promptly to healthcare providers.
Nail changes as early warning signs
Among the most valuable early indicators of psoriatic arthritis are changes to the fingernails and toenails. Nearly 80 percent of people with PsA develop nail abnormalities that can appear before other joint symptoms.
These changes include pitting (small depressions in the nail surface), onycholysis (separation of the nail from the nail bed), thickening, and discoloration. The close anatomical relationship between the nails and the small joints of the fingers and toes explains why nail changes often signal the beginning of joint inflammation.
For healthcare providers, distinctive nail changes in someone with psoriasis raise immediate concern about developing psoriatic arthritis. Regular examination of the nails can serve as an early detection method for people with psoriasis or a family history of these conditions.
Fatigue and its impact on daily life
Beyond the visible symptoms of skin and joint inflammation, many people with psoriatic arthritis experience profound fatigue that significantly affects their quality of life. This exhaustion stems from several factors, including the body’s inflammatory response, disrupted sleep due to pain, and the psychological burden of managing a chronic condition.
The fatigue associated with PsA often feels different from ordinary tiredness. Many describe it as a heavy, persistent exhaustion that isn’t relieved by rest or sleep. This symptom can appear before diagnosis and sometimes fluctuates with disease activity, becoming more severe during flare-ups.
For many, this fatigue represents one of the most challenging aspects of living with psoriatic arthritis, affecting work performance, family responsibilities, and social engagements. Healthcare providers increasingly recognize fatigue as a core symptom requiring specific management strategies beyond just treating joint inflammation.
Eye inflammation complications
Approximately 7 percent of individuals with psoriatic arthritis develop uveitis, an inflammatory eye condition that requires immediate attention. This inflammation affects the middle layer of tissue in the eye wall and can lead to permanent vision damage if left untreated.
Symptoms include eye pain, redness, sensitivity to light, and blurred vision. These eye problems stem from the same inflammatory processes that affect the joints and skin, highlighting PsA’s nature as a systemic inflammatory condition.
Regular eye examinations become particularly important for those diagnosed with psoriatic arthritis, as early intervention for uveitis can prevent long-term complications. Any sudden changes in vision or eye discomfort warrant prompt medical evaluation.
Diagnosis challenges and approaches
Diagnosing psoriatic arthritis presents challenges because no single test can confirm its presence. Healthcare providers typically follow a comprehensive approach that begins with a thorough medical history and physical examination.
The diagnostic process usually includes blood tests to check for inflammatory markers like C-reactive protein and erythrocyte sedimentation rate. While these tests cannot confirm PsA specifically, they help assess inflammation levels in the body. Additionally, rheumatoid factor tests often return negative in PsA patients, helping distinguish it from rheumatoid arthritis.
Imaging plays a crucial role in diagnosis. X-rays can reveal changes in the joints characteristic of PsA, such as pencil-in-cup deformities where the end of a bone resembles a pencil fitting into a cup-shaped socket. For earlier detection, magnetic resonance imaging (MRI) proves more sensitive, showing inflammation in joints and tendons before damage appears on X-rays.
Classification criteria developed by the Classification Criteria for Psoriatic Arthritis (CASPAR) help standardize diagnosis. These criteria include current psoriasis, personal or family history of psoriasis, typical nail changes, negative rheumatoid factor, and evidence of dactylitis.
Early diagnosis remains critical, as joint damage can occur within the first two years of disease onset. The earlier treatment begins, the better the long-term outcomes in terms of joint function and quality of life.
Treatment advances and strategies
Treatment for psoriatic arthritis has evolved significantly in recent years, offering new hope for patients. The goals of therapy include reducing inflammation, relieving pain, preventing joint damage, and controlling skin symptoms.
Non-steroidal anti-inflammatory drugs (NSAIDs) often serve as first-line treatments for mild cases, helping manage pain and reduce inflammation. For those with more severe disease, disease-modifying antirheumatic drugs (DMARDs) like methotrexate work to slow disease progression and prevent joint destruction.
The most significant advances have come with biologic medications, which target specific components of the immune system involved in inflammation. Tumor necrosis factor (TNF) inhibitors, interleukin-17 inhibitors, and interleukin-23 inhibitors have transformed treatment by providing more precise approaches to controlling the disease.
Janus kinase (JAK) inhibitors represent another innovative class of medications that block pathways involved in the inflammatory process. These oral medications offer alternatives for patients who don’t respond adequately to or cannot tolerate other treatments.
For some individuals, a combination of therapies proves most effective. This comprehensive approach might include medications, physical therapy to maintain joint function, occupational therapy to adapt daily activities, and exercise programs specifically designed for people with arthritis.
Lifestyle management and self-care
Beyond medical treatments, lifestyle factors significantly influence psoriatic arthritis management. Maintaining a healthy weight reduces stress on joints and may improve response to medications, as excess fat tissue produces inflammatory substances that can worsen PsA.
Regular, appropriate exercise helps preserve joint function and mobility. Low-impact activities like swimming, walking, and cycling provide cardiovascular benefits without placing excessive stress on inflamed joints. Working with physical therapists to develop personalized exercise programs ensures safety and effectiveness.
Diet choices may also influence disease activity. While no specific diet has been proven to treat PsA, anti-inflammatory eating patterns like the Mediterranean diet, rich in fruits, vegetables, whole grains, fish, and olive oil, may help reduce overall inflammation.
Stress management techniques such as mindfulness meditation, deep breathing exercises, and yoga can help modulate the immune response and improve coping skills. Many find that stress triggers or worsens flares, making stress reduction an important component of self-care.
Protecting joints during daily activities, using assistive devices when necessary, and making ergonomic adjustments at home and work can prevent additional strain on affected joints. These practical approaches complement medical treatment and enhance overall function.
Future research directions
Research into psoriatic arthritis continues to advance understanding of this complex condition. Current investigations focus on identifying biomarkers that could predict which psoriasis patients will develop PsA, potentially allowing for preventive interventions.
Genetic studies aim to unravel the hereditary components of the disease, which could lead to more personalized treatment approaches based on individual genetic profiles. The discovery of new molecular targets involved in the inflammatory cascade promises even more precise therapies in the future.
Clinical trials exploring combination therapies, optimal treatment sequencing, and strategies for tapering medications once remission is achieved offer hope for more effective and streamlined treatment protocols. Additionally, research into the microbiome – the collection of microorganisms living in and on the human body – suggests potential connections to PsA development and progression.
With continued research and growing awareness, the outlook for people with psoriatic arthritis continues to improve. Early recognition, prompt treatment, and comprehensive care offer the best chance for managing this challenging condition and maintaining quality of life.