How informed advocacy and community resources are transforming asthma care
The health summit stage grew quiet as a mother described equipping her infant’s car seat with portable oxygen tanks—a routine necessity in her family’s battle against severe childhood asthma. Her story represents thousands of African American families navigating a troubling health reality: Black children face asthma rates twice as high as their white peers, with mortality rates eight times greater.
This dramatic disparity persists despite medical advances, highlighting how systemic barriers continue shaping health outcomes across communities. At the recent BHM 2025 Spring Health Summit, the conversation moved beyond statistics to explore practical strategies for families confronting these challenges.
For many African American families, managing childhood asthma requires extraordinary vigilance, healthcare navigation skills, and persistence against a system not always responsive to their needs. Yet across the country, determined caregivers are developing effective approaches to protect their children’s health and transform asthma care within their communities.
The hidden burden: Asthma’s unequal impact
The statistics paint a concerning picture of health inequality. According to the U.S. Department of Health and Human Services Office of Minority Health, non-Hispanic Black children are twice as likely to develop asthma compared to non-Hispanic white children. The Centers for Disease Control and Prevention notes Black individuals face 40% higher asthma rates overall, with Black children experiencing dramatically higher mortality from asthma-related complications.
These disparities stem from multiple interconnected factors. African American families disproportionately reside in areas with higher environmental pollutants, substandard housing conditions, and proximity to industrial zones—all known asthma triggers. Limited access to preventive care and specialists further compounds these environmental challenges.
The economic impact adds another layer of difficulty. Asthma-related hospitalizations, emergency visits, and missed school days create financial strain through medical bills and lost work hours for caregivers. This economic burden reinforces health disparities, creating a challenging cycle for many families.
Despite these obstacles, communities are developing innovative approaches to asthma management, combining medical care with advocacy, education, and environmental interventions.
Recognizing early signs: Beyond typical symptoms
Early recognition of asthma symptoms in children remains crucial but challenging, especially when presentations differ from textbook descriptions. While wheezing and shortness of breath are well-known indicators, parents should also watch for persistent coughing (especially at night), recurring respiratory infections, and unusual fatigue after physical activity.
In infants and very young children, symptoms might include rapid breathing, flaring nostrils during breathing, or visible retractions—the skin pulling in around the ribs or neck with each breath. Parents who notice these patterns should document them carefully to share with healthcare providers, as early intervention significantly improves outcomes.
For children born prematurely, asthma risk increases substantially. These children often require special monitoring throughout early childhood, with particular attention to respiratory health during seasonal transitions and virus outbreaks. Tracking patterns helps identify triggers and develop personalized management plans.
Some parents report encountering dismissive attitudes when reporting these symptoms, particularly in emergency or urgent care settings. Preparing detailed observations about frequency, duration, and circumstances of symptoms helps validate concerns and advocate for appropriate evaluation.
Navigating healthcare: Building an effective medical team
Finding responsive, culturally competent healthcare providers represents a critical step in managing childhood asthma effectively. Families report that the ideal asthma care team includes not just specialists but providers who listen attentively, respect parental observations, and collaborate on treatment plans.
Establishing a consistent relationship with primary care providers creates continuity in asthma management. This ongoing relationship helps track patterns over time and adjust treatments before emergencies occur. For many families, pediatricians serve as the cornerstone of this care, coordinating with specialists when needed.
Pulmonologists and allergists provide specialized expertise in complex cases. While referrals to these specialists sometimes face insurance barriers or long wait times, their involvement often proves transformative in developing comprehensive treatment plans. Families can request referrals persistently if initial symptoms aren’t adequately controlled with primary care interventions.
Community health centers increasingly offer asthma management programs designed for underserved populations. These programs often include care coordinators who help families navigate appointment systems, medication access, and insurance issues—removing practical barriers to consistent care.
Parents who encounter healthcare bias must develop effective advocacy strategies. These include seeking second opinions, bringing support persons to appointments, documenting all symptoms and triggers methodically, and when necessary, requesting different providers within the same practice.
Educational advocacy: Securing school support
For children with asthma, school environments present both challenges and opportunities. Educational advocacy ensures children receive appropriate accommodations while accessing their education fully. This process often begins with securing formal documentation through medical providers.
Asthma action plans serve as critical documents that outline symptoms, medications, and emergency protocols. These plans should be shared with school nurses, teachers, coaches, and administrative staff. Updated copies should be provided at the beginning of each school year and whenever treatment changes occur.
For children with severe asthma, Individualized Education Programs (IEPs) or 504 plans provide formal accommodations. These might include modified physical education requirements, permission to carry rescue inhalers, arrangements for missed work during hospitalizations, or environmental modifications in classrooms.
School nurses play vital roles in asthma management, administering medications and monitoring symptoms during school hours. Building collaborative relationships with these professionals helps ensure prompt recognition of early warning signs. In schools without full-time nurses, parents may need to advocate for training additional staff members.
Environmental assessments of school buildings can identify potential asthma triggers like mold, pest infestations, or poor ventilation. Parents can request these assessments individually or collectively through parent organizations. The EPA’s Tools for Schools program provides resources for addressing indoor air quality issues in educational settings.
Environmental management: Controlling triggers at home
While medical treatment remains essential, environmental management significantly reduces asthma attacks. Understanding and controlling triggers in the home environment represents a powerful, though sometimes challenging, approach to asthma management.
Common household triggers include dust mites, pet dander, cockroach allergens, rodent allergens, mold, and secondhand smoke. Identifying specific triggers through allergy testing helps families prioritize environmental interventions most relevant to their situation.
Basic interventions include using allergen-proof mattress and pillow covers, washing bedding weekly in hot water, removing carpeting when possible, reducing clutter that collects dust, and maintaining humidity levels below 50% to prevent mold growth.
Addressing structural issues often presents greater challenges, particularly for renters or those in older housing. Water leaks, inadequate ventilation, and pest infestations require cooperation from property owners. Several nonprofit organizations now assist families in documenting these conditions and understanding their legal rights to habitable housing.
Community resources increasingly focus on home environmental assessments. Programs through local health departments, nonprofit organizations, and some insurance plans offer home visits to identify specific triggers and recommend targeted interventions. These programs sometimes provide HEPA vacuum cleaners, air purifiers, and integrated pest management services.
Medication management: Ensuring consistent treatment
Effective asthma control requires consistent medication management, often involving both maintenance and rescue medications. Understanding the difference between these medication types—and ensuring reliable access to both—forms the foundation of daily asthma care.
Controller medications (typically inhaled corticosteroids) reduce airway inflammation when used regularly, even without symptoms present. These preventive medications require daily administration to maintain effectiveness. Some families report discontinuing these medications when symptoms improve, not realizing this increases risk of future attacks.
Rescue medications provide immediate relief during asthma symptoms but don’t address underlying inflammation. Tracking frequency of rescue medication use helps identify when asthma control is slipping—using rescue inhalers more than twice weekly generally indicates the need for adjusted treatment plans.
Medication adherence faces several barriers, including insurance coverage gaps, pharmacy stock issues, and complex administration techniques. Community pharmacists can provide technique training, medication calendars, and sometimes emergency supplies when insurance authorizations delay refills.
Patient assistance programs offered by pharmaceutical manufacturers help address financial barriers for both insured and uninsured families. These programs require application processes that community health workers or social workers can often assist with navigating.
Community resources: Accessing specialized support
Across the country, community organizations have developed specialized programs addressing asthma disparities in African American communities. These resources offer education, environmental interventions, and emotional support beyond traditional medical care.
The Asthma and Allergy Foundation of America (AAFA) provides educational materials specifically designed for diverse communities, including resources addressing cultural beliefs about asthma. Their website offers downloadable action plans, trigger management guides, and connections to local support groups.
Breathe DC and similar regional organizations conduct home environmental assessments, provide HEPA vacuum cleaners, and offer integrated pest management services. These organizations often employ community health workers from the neighborhoods they serve, increasing cultural competence in service delivery.
Black church health ministries increasingly incorporate asthma education into their programming, recognizing the condition’s prevalence within their congregations. These faith-based initiatives combine practical information with spiritual support, addressing both physical and emotional aspects of chronic illness management.
Asthma camps provide children opportunities to learn self-management skills while enjoying typical childhood experiences in medically supervised environments. Many camps offer scholarships specifically for children from underserved communities, though availability varies by region.
Advocacy efforts: Driving systemic change
While individual management strategies remain essential, broader advocacy efforts address systemic factors perpetuating asthma disparities. Community organizing around environmental justice, healthcare access, and housing quality creates long-term improvements benefiting entire neighborhoods.
Environmental justice campaigns focus on reducing industrial emissions in predominantly Black neighborhoods, enforcing existing air quality regulations, and requiring health impact assessments before new facility construction. These efforts directly address external triggers affecting entire communities.
Housing advocacy targets code enforcement, tenant rights, and healthy housing standards. Organizations in several cities have successfully established “asthma-friendly” housing certification programs that incentivize landlords to address common triggers like mold remediation and pest management.
School-focused initiatives work toward comprehensive indoor air quality assessments, removing asthma triggers from educational environments, and establishing consistent policies for medication access during school hours. These efforts benefit all students while particularly protecting those with existing respiratory conditions.
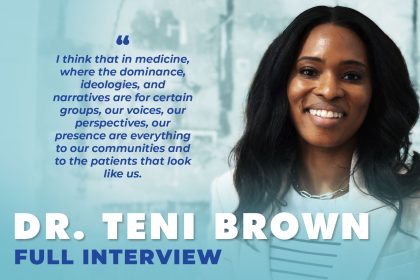
Healthcare advocacy addresses insurance coverage gaps, specialist access, and cultural competence in medical education. Community review boards increasingly provide input on research priorities and healthcare delivery models, ensuring interventions address community-identified needs rather than researcher assumptions.
Building resilience: The emotional journey
The emotional toll of managing childhood asthma receives less attention than medical aspects but significantly impacts family wellbeing. Parents report experiencing anxiety, hypervigilance, and sometimes guilt related to their children’s condition, particularly following severe attacks or hospitalizations.
Peer support groups offer safe spaces to process these emotions and share practical coping strategies. Some hospital systems now facilitate connections between families facing similar challenges, recognizing that shared experience provides unique understanding.
Children with asthma may experience fear, frustration with activity limitations, or discomfort with appearing “different” from peers. Age-appropriate education about their condition helps children develop self-management skills and confidence in handling symptoms.
Resilience-building approaches focus on identifying strengths within challenging situations. Families report that becoming knowledgeable advocates transforms their relationship with medical systems and enhances their sense of agency in protecting their children’s health.
Community celebrations of “asthma champions”—children effectively managing their conditions while pursuing their interests—provide powerful counter-narratives to deficit-focused discussions of health disparities. These stories inspire other families while recognizing children’s courage in facing chronic health challenges.
Looking forward: A framework for progress
Progress in addressing asthma disparities requires multilevel approaches combining medical care, environmental interventions, community resources, and policy changes. The most effective models integrate these elements into comprehensive asthma management programs.
Medical institutions increasingly adopt team-based approaches including community health workers who bridge clinical care and home environments. These programs show promising results in reducing emergency department visits and hospitalizations while improving quality of life.
School-based health centers provide accessible care within educational settings, reducing barriers related to transportation and parent work schedules. These centers combine direct services with classroom education about asthma triggers and management strategies.
Technology innovations including smartphone-connected inhalers, air quality monitoring applications, and telemedicine follow-up after emergency visits expand management options. Ensuring equitable access to these technologies remains an important consideration in their implementation.
Policy approaches addressing underlying determinants of health include expanding Medicaid coverage, enforcing housing quality standards, and reducing air pollution in vulnerable communities. These structural interventions create conditions where individual management strategies can succeed.
The path forward requires sustained commitment from healthcare providers, community organizations, policymakers, and families themseles. By combining medical expertise with community wisdom, meaningful progress becomes possible in addressing one of the most persistent health disparities affecting African American children.
For families currently navigating childhood asthma challenges, the most important message remains one of hope through practical action: With appropriate care, environmental management, and advocacy, children with asthma can participate fully in school, sports, and social activities while developing the skills to manage their health effectively throughout life.