The waiting room is packed. The doctor is running two hours behind. The bill will make your eyes water. And that’s if you’re lucky enough to get an appointment at all. But while health care remains a frustrating, expensive maze for most Americans, artificial intelligence is quietly revolutionizing how, when, and where we access medical care — potentially solving problems that have seemed impossible for decades.
The diagnostic democratization
One of the most transformative applications of AI in health care is its ability to bring sophisticated diagnostic tools to underserved populations. Algorithms that can spot pneumonia on chest X-rays, detect diabetic retinopathy from eye scans, or identify skin cancers from photographs are extending the reach of specialist-level diagnostics beyond urban medical centers.
This means the expertise once confined to major hospitals can now reach rural clinics, community health centers, and eventually even smartphones. In areas facing physician shortages, AI tools are helping nurses, physician assistants, and general practitioners deliver care that previously required specialists who simply weren’t available locally.
This geographic barrier-breaking is particularly significant for the roughly 20 percent of Americans living in rural areas, where the nearest specialist might be hours away. When AI can help a local provider diagnose a condition that would typically require a distant referral, it saves patients not just money but precious time — often the difference between catching a condition early or discovering it too late.
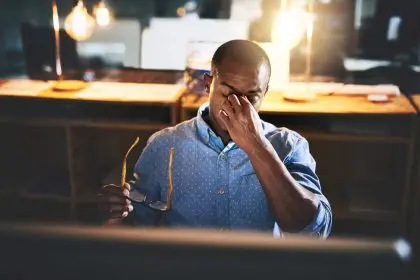
The waiting room revolution
The days of sitting in waiting rooms for hours might be numbered thanks to AI triage systems that are fundamentally changing how we decide who needs in-person care and when. These systems range from sophisticated symptom checkers to chatbots that gather medical histories before appointments.
What makes these tools particularly powerful is their ability to learn from millions of patient interactions and outcomes, becoming increasingly accurate at distinguishing between conditions requiring immediate attention and those that can safely wait or be handled remotely. This means fewer unnecessary emergency room visits, shorter waits for those who truly need urgent care, and more efficient use of limited medical resources.
The impact is particularly meaningful for people with limited transportation options, inflexible work schedules, or childcare responsibilities — often the same populations that already face the greatest health care barriers. When an AI system can confidently tell you whether your symptoms warrant a trip to the emergency room or can wait for a telehealth appointment, it removes the guesswork that leads many people to either delay necessary care or spend hours waiting for reassurance they didn’t need.
The language barrier breakthrough
For the roughly 25 million Americans with limited English proficiency, navigating the health care system presents an additional layer of complexity. Traditional translation services are expensive, often unavailable for less common languages, and frequently create delays in care delivery. AI-powered real-time translation is changing this landscape dramatically.
These systems can now translate medical conversations with remarkable accuracy, including the specialized terminology that trips up general translation tools. More advanced versions even account for cultural nuances in how symptoms are described across different languages, helping providers understand not just the words but the meaning behind them.
This technology means more accurate diagnoses, better adherence to treatment plans, and significantly improved patient experiences for immigrant communities. When patients can communicate directly with providers in their native language, they’re more likely to share complete information, understand their treatment options, and follow through on recommendations — all critical factors in successful health care outcomes.
The monitoring mobilization
AI is fundamentally changing how chronic conditions are managed by enabling sophisticated remote monitoring that once required hospital stays or frequent clinic visits. From diabetes to heart failure to high-risk pregnancies, algorithm-powered monitoring systems are keeping people healthier at home while drastically reducing costs.
These systems combine wearable devices or simple home testing kits with AI that can detect subtle patterns indicating potential problems. What makes them revolutionary is their ability to identify concerning trends before they become medical emergencies, allowing for preventive interventions rather than crisis responses.
For people with mobility challenges, transportation barriers, or complex conditions that make frequent medical visits difficult, these monitoring systems offer unprecedented access to continuous care. They’re particularly transformative for elderly patients, for whom a trip to the doctor’s office might require significant assistance, and for whom early intervention can prevent common but dangerous complications.
The mental health makeover
Perhaps nowhere is the accessibility impact of AI more profound than in mental health care, where provider shortages have reached crisis levels. With wait times for psychiatrists often stretching to months, AI-powered tools are filling critical gaps in the mental health treatment landscape.
These range from therapeutic chatbots that provide evidence-based cognitive behavioral therapy to sentiment analysis systems that can detect signs of depression or suicidal ideation from text messages. While not replacements for human therapists, these tools are providing support during wait periods and extending care between sessions.
For the millions of Americans living in mental health professional shortage areas — now more than 60 percent of U.S. counties — these tools offer access to evidence-based therapeutic approaches that would otherwise be completely unavailable. They’re particularly valuable for people hesitant to seek in-person mental health care due to stigma, cost concerns, or privacy preferences.
The cost containment catalyst
Health care costs remain the leading cause of bankruptcy in America, with even insured patients facing devastating bills for necessary care. AI is tackling this accessibility barrier through sophisticated cost prediction and reduction tools that make health care more financially manageable.
By analyzing millions of claims and outcomes, AI systems can identify equally effective but less expensive treatment pathways, predict which patients might benefit from preventive interventions to avoid costly complications, and streamline administrative processes that drive up costs without improving care.
Some of the most promising applications help patients understand their actual out-of-pocket costs before receiving care — a level of transparency that’s been notoriously absent from American health care. When patients can see accurate cost estimates for different treatment options and facilities, they can make informed decisions that avoid financial catastrophe while still addressing their medical needs.
The prevention pivot
Perhaps the most profound way AI is making health care more accessible is by helping shift resources from expensive crisis interventions to more affordable and effective preventive care. By identifying high-risk individuals before they develop serious conditions, these systems enable targeted prevention programs that are both more accessible and more cost-effective than treating advanced disease.
AI risk prediction models can incorporate thousands of factors — from genetic information to social determinants of health — to identify who might benefit most from specific preventive services. This allows health care systems to proactively reach out to vulnerable populations rather than waiting for them to overcome access barriers on their own.
This shift is particularly significant for communities that have historically received reactive rather than proactive health care. When prevention resources are targeted based on sophisticated risk analysis rather than who shows up at the doctor’s office, they naturally flow more equitably to populations that traditional health care systems have often failed to serve adequately.
The administrative reduction
The byzantine paperwork requirements of American health care create substantial accessibility barriers, particularly for people with limited time, English proficiency, or health literacy. AI is dramatically reducing this burden through intelligent automation of administrative processes.
From eligibility verification for assistance programs to automated prior authorization for treatments, these systems are eliminating paperwork obstacles that prevented many people from accessing care they were entitled to receive. The impact is particularly meaningful for complex programs like Medicaid, where eligibility rules and documentation requirements have historically deterred eligible individuals from enrolling or maintaining coverage.
By reducing the administrative knowledge required to navigate the health care system, these tools effectively make care more accessible to people without health care backgrounds, advanced education, or significant free time to manage paperwork — often the same populations with the greatest unmet health care needs.
The equity enhancer
Health care disparities along racial, geographic, and socioeconomic lines have proven stubbornly resistant to traditional interventions. AI tools, thoughtfully designed and implemented, offer new approaches to identifying and addressing these gaps.
By analyzing patterns in care delivery and outcomes across different populations, AI systems can highlight disparities that might otherwise remain invisible within massive health care datasets. More importantly, they can help identify the specific barriers driving these disparities and suggest targeted interventions to address them.
This data-driven approach to health care equity means resources can be directed precisely where they’ll have the greatest impact on accessibility, rather than relying on one-size-fits-all solutions that often fail to reach the most vulnerable populations. When combined with AI tools that extend care beyond traditional settings, this targeted approach is creating unprecedented access for communities historically underserved by the health care system.
The practical limitations
Despite its transformative potential, AI isn’t a magic solution to all health care accessibility challenges. Broadband access remains limited in many rural areas, creating a digital divide that can actually widen disparities if AI tools primarily require high-speed internet. Similarly, many promising applications require smartphones or other devices that aren’t universally available across socioeconomic groups.
There are also legitimate concerns about algorithmic bias, particularly for tools trained on datasets that underrepresent certain populations. When an AI system hasn’t been exposed to diverse training data, it may perform less effectively for minority groups — potentially worsening rather than improving health care disparities.
These limitations highlight the importance of thoughtful implementation strategies that consider the full spectrum of accessibility barriers. The most successful approaches combine AI technologies with human support systems, ensuring these powerful tools extend rather than replace the human connections that remain essential to effective health care.