The science behind GLP-1 medications and how they work
GLP-1 receptor agonists operate by mimicking a natural hormone that regulates blood sugar, slows digestive processes, and signals fullness to the brain. This multi-faceted approach explains why these medications have become increasingly popular for both diabetes management and weight loss treatments.
These medications work through several mechanisms simultaneously. They slow stomach emptying, which helps you feel fuller longer after eating. They regulate blood glucose by stimulating insulin release when blood sugar rises. Additionally, they act on brain receptors that control appetite and food cravings, reducing hunger sensations and potentially decreasing interest in highly palatable foods.
The two most prominent medications in this category include semaglutide (available as Wegovy for weight management and Ozempic for diabetes) and tirzepatide (marketed as Zepbound for weight loss and Mounjaro for diabetes). While they share core mechanisms, important differences exist between them that may explain varying patient experiences.
Semaglutide functions as a single-action GLP-1 receptor agonist, specifically targeting the GLP-1 pathway. In contrast, tirzepatide employs a dual-action approach, activating both GLP-1 receptors and glucose-dependent insulinotropic polypeptide (GIP) receptors. This additional pathway may contribute to different side effect profiles and potentially enhanced effectiveness for some patients.
Common side effects that impact quality of life
Gastrointestinal issues dominate the side effect profile of GLP-1 medications, with nausea being particularly prevalent. This nausea typically results from the medication’s intentional slowing of stomach emptying, which can create feelings of fullness that sometimes transition into queasiness.
Beyond nausea, many patients experience acid reflux or heartburn, especially in the early weeks of treatment. The delayed stomach emptying can increase pressure in the stomach, forcing acid back into the esophagus. This symptom often appears or worsens after meals, particularly following larger or higher-fat food choices.
Constipation affects approximately 30% of GLP-1 medication users, resulting from slower digestive transit and potentially decreased fluid intake due to reduced appetite. This side effect can become particularly uncomfortable if not proactively addressed with adequate hydration and dietary fiber.
Many patients also report significant appetite suppression that extends beyond normal fullness to actual disinterest in food. While beneficial for weight loss goals, this effect can sometimes lead to inadequate nutrition if not carefully monitored, particularly regarding protein intake necessary for maintaining muscle mass during weight loss.
Less commonly discussed but still significant are symptoms like fatigue, headaches, and mild dizziness that some patients experience, particularly during dose increases. These effects may relate to changes in caloric intake, fluid balance, or the body’s adaptation to altered metabolic processes.
Why your body might react differently than others
Individual responses to GLP-1 medications vary substantially based on several biological and lifestyle factors that influence how these drugs affect the body’s systems.
Genetic differences play a significant role in medication response. Variations in genes affecting drug metabolism, receptor sensitivity, and gastrointestinal function can substantially impact both effectiveness and side effects. These genetic factors help explain why even siblings might have dramatically different experiences with the same medication.
Body composition factors into response patterns as well. People with higher initial body weights or different fat distribution patterns may process these medications differently. Some research suggests that those with higher visceral fat (fat around the organs) might experience more pronounced initial side effects but potentially greater long-term benefits.
Previous medication history influences how your body adapts to GLP-1 drugs. Those who have used other medications affecting digestion or appetite may have partially primed digestive systems or neural pathways, potentially altering their response to these newer medications.
Dietary patterns significantly impact side effect intensity. High-fat meals tend to exacerbate nausea and reflux symptoms with GLP-1 medications, while protein-rich, moderate-fat meals are often better tolerated. Your typical eating patterns before starting medication may predict your adjustment experience.
Stress levels and sleep quality also affect medication response. Higher stress or disrupted sleep can amplify side effects through their impact on digestive function and sensitivity to discomfort. Those with existing stress-related digestive issues may notice more pronounced effects initially.
Strategies to minimize uncomfortable side effects
Successful management of GLP-1 medication side effects typically involves a combination of dosing strategies, dietary adjustments, and lifestyle modifications tailored to individual needs.
Starting with lower doses than prescribed and gradually increasing is a common approach endorsed by many healthcare providers. This “low and slow” method allows your body to adjust incrementally, potentially reducing side effect intensity. Always discuss this approach with your healthcare provider rather than modifying dosing independently.
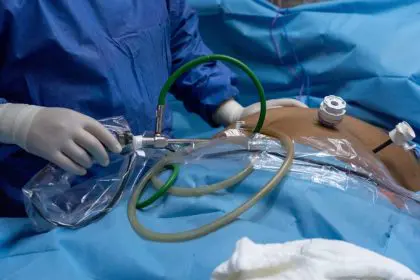
Timing medication administration strategically can significantly impact tolerance. Taking the injection before bedtime works well for some patients, allowing them to sleep through the peak hours of potential nausea. Others find morning administration followed by a light, protein-focused breakfast offers better overall daily tolerance.
Dietary modifications represent perhaps the most effective side effect management strategy. Smaller, more frequent meals prevent the stomach from becoming too empty or too full—both states that can trigger nausea with these medications. Avoiding very fatty, spicy, or highly processed foods can further reduce digestive distress.
Hydration requires particular attention during GLP-1 treatment. Reduced thirst sensations often accompany appetite suppression, potentially leading to dehydration that worsens constipation and other side effects. Setting regular hydration reminders and keeping water visible and accessible throughout the day helps maintain adequate fluid intake.
Anti-nausea supplements and medications provide additional options for managing persistent symptoms. Ginger supplements or tea, vitamin B6, and prescription anti-nausea medications can be helpful for those experiencing significant discomfort. Always consult your healthcare provider before adding any supplements or medications to your regimen.
When to consider switching medications
Despite best management efforts, some patients ultimately determine that switching between GLP-1 medications offers a better solution for their particular situation and health goals.
Persistent severe side effects that significantly impact quality of life despite appropriate management strategies represent the most common reason for medication changes. If nausea, vomiting, or other symptoms remain severe after several weeks of consistent use and side effect management techniques, discussing alternatives becomes appropriate.
Inadequate effectiveness despite reaching target dosage sometimes necessitates reconsideration of medication choice. Different GLP-1 medications and formulations have varying potencies and mechanisms, meaning some patients respond better to one option than another. This variability partly explains why approximately 11% of patients switch between these medications.
Insurance coverage and cost considerations often influence medication decisions as well. Coverage for specific GLP-1 medications varies widely between insurance plans, sometimes making one option substantially more affordable than another. Since these treatments typically continue long-term, cost sustainability remains an important consideration.
Personal preference regarding dosing frequency also affects medication choice. Semaglutide requires weekly injections, while some patients prefer the daily administration of certain other options in this drug class, finding it easier to remember or better aligned with their routines.
When considering medication changes, healthcare providers typically recommend completing at least 4-8 weeks on the initial medication when possible, allowing sufficient time for side effects to stabilize and true effectiveness to become apparent before making switches.
Working with your healthcare provider for personalized treatment
The relationship with your healthcare provider plays a crucial role in successful GLP-1 medication management, as individualized approaches typically yield the best outcomes.
Regular monitoring through follow-up appointments allows tracking of both progress and side effects, enabling timely adjustments to dosage or medication type. These appointments should include weight measurements, discussion of side effects, and assessment of overall well-being and quality of life while on treatment.
Comprehensive blood work helps ensure the medication isn’t causing unexpected metabolic effects and confirms that nutritional status remains adequate despite appetite changes. Regular testing of kidney function, thyroid levels, and other metabolic markers provides important safety monitoring during treatment.
Open communication about all symptoms—not just the expected side effects—helps identify potential concerns early. Some patients hesitate to mention digestive issues, assuming they must simply tolerate them as part of treatment. However, healthcare providers can often suggest simple modifications that significantly improve comfort.
Setting realistic expectations remains essential for sustainable treatment. Understanding that some initial side effects are normal but typically improve over time helps patients persist through adjustment periods. Equally important is recognizing that weight loss typically occurs gradually, with initial rapid losses often moderating over time.
Discussing complementary approaches such as nutritional counseling, behavioral support, or physical activity guidance creates a more holistic treatment plan. These additional interventions not only enhance medication effectiveness but often help minimize side effects through improved overall health.
The future of GLP-1 treatments and emerging options
The landscape of GLP-1 medications continues evolving rapidly, with new formulations and combination therapies promising potentially improved effectiveness and tolerability.
Oral formulations of GLP-1 medications represent a significant advancement currently in development. These options could eliminate the need for injections, potentially increasing treatment accessibility and acceptability for patients hesitant about self-injecting medication.
Combination therapies pairing GLP-1 medications with other weight management agents show promising early results. These approaches target multiple pathways simultaneously, potentially offering greater effectiveness than single-agent treatments while possibly reducing side effects through lower individual drug dosages.
Extended-release formulations requiring less frequent administration are under investigation. Monthly injection options could improve convenience and adherence compared to current weekly regimens, potentially enhancing long-term treatment success rates.
Personalized medicine approaches using genetic testing to predict medication response represent an exciting frontier in obesity treatment. Future protocols might use individual genetic profiles to determine which specific GLP-1 medication would likely provide optimal effectiveness with minimal side effects for each patient.
As research continues advancing our understanding of these medications, treatment protocols will likely become increasingly refined and individualized. The growing recognition that obesity represents a chronic medical condition requiring long-term management approaches continues driving innovation in this rapidly evolving field.
By understanding the reasons behind varying responses to GLP-1 medications and implementing appropriate management strategies, patients can maximize benefits while minimizing discomfort. Working closely with healthcare providers to find the right medication and management approach for your unique situation offers the best path toward successful treatment outcomes and improved health.