Tuberculosis remains one of the world’s most persistent infectious diseases, affecting millions annually despite significant medical advances. This bacterial infection primarily targets the lungs but can spread to other organs when left untreated. Early recognition of warning signs dramatically improves treatment outcomes and prevents transmission to family members and communities.
The challenge with tuberculosis lies in its subtle onset and gradual progression. Many people dismiss initial symptoms as common cold or flu, allowing the infection to establish deeper roots in the respiratory system. Understanding these nine critical warning signs empowers individuals to seek timely medical evaluation and begin appropriate treatment before complications arise.
Modern tuberculosis presents differently than historical accounts might suggest. While the disease once carried a death sentence, contemporary medical interventions offer excellent cure rates when detected early. However, delayed diagnosis can lead to severe complications, drug resistance, and increased transmission risk to close contacts.
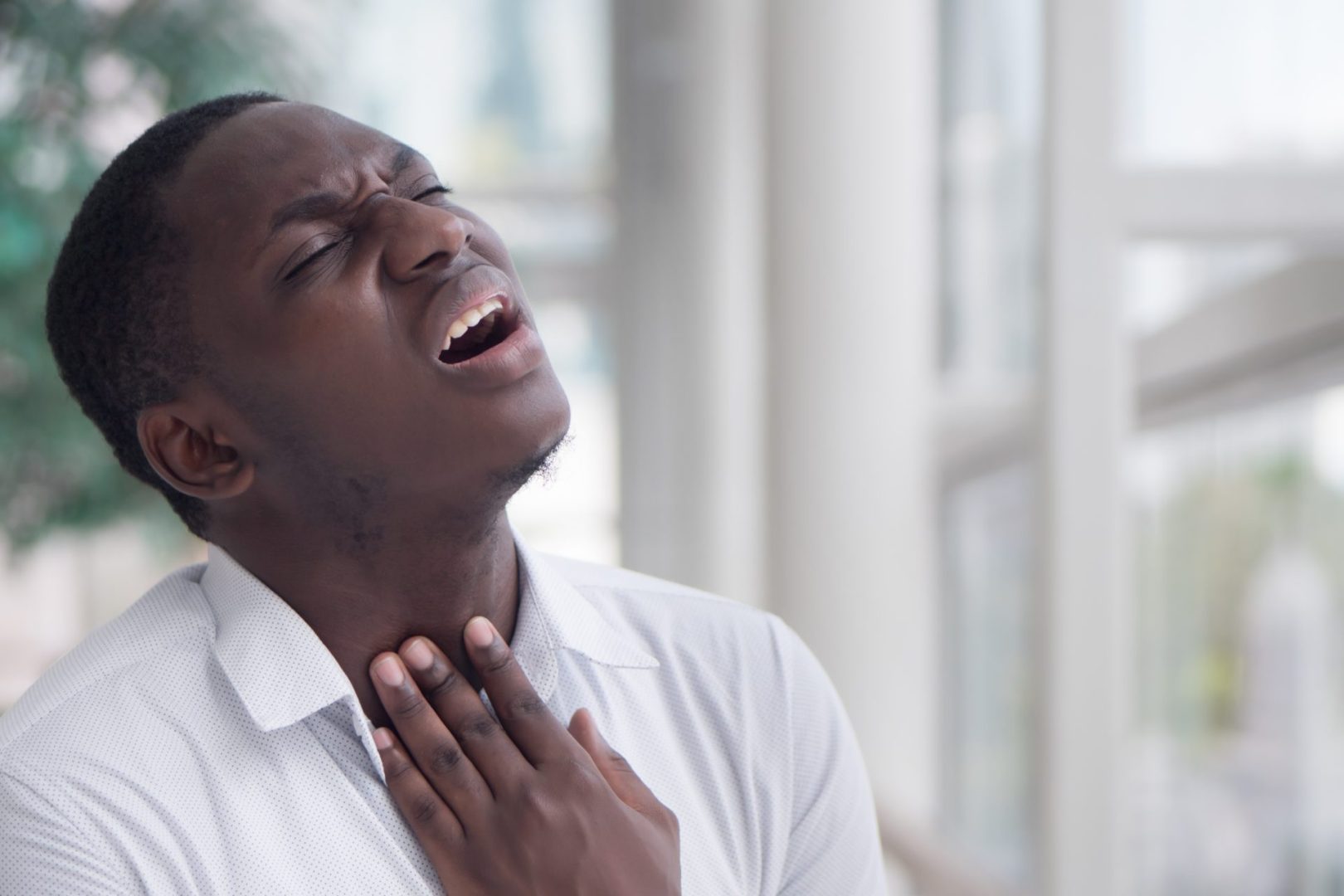
1. Persistent cough lasting more than three weeks
A chronic cough represents the most common early indicator of pulmonary tuberculosis. Unlike typical respiratory infections that resolve within days or weeks, tuberculosis-related coughing persists and often worsens over time. This cough typically produces phlegm or sputum, distinguishing it from dry coughs associated with other conditions.
The tuberculosis cough often begins as a mild irritation that gradually intensifies. Initially, it may occur primarily in the morning or evening, but progression leads to frequent coughing throughout the day and night. The persistent nature stems from ongoing lung tissue inflammation caused by bacterial multiplication and immune system response.
Sputum production increases as the infection progresses, transitioning from clear or white to yellow, green, or rust-colored. The changing appearance reflects increased bacterial load and tissue damage within the respiratory system. Blood-tinged sputum, while alarming, indicates significant lung involvement requiring immediate medical attention.
Many people attempt to suppress this cough with over-the-counter medications, inadvertently masking an important diagnostic clue. The ineffectiveness of standard cough suppressants against tuberculosis-related coughing should prompt medical evaluation rather than continued self-treatment attempts.
2. Unexplained weight loss and appetite changes
Tuberculosis significantly impacts metabolism and nutritional status, leading to progressive weight loss despite maintained or increased caloric intake. This weight reduction often occurs gradually, making it less noticeable until clothing becomes loose or others comment on physical changes.
The bacterial infection increases metabolic demands while simultaneously reducing appetite and nutrient absorption. Chronic inflammation consumes energy reserves, while toxins produced by tuberculosis bacteria interfere with normal digestive processes. This combination creates a negative energy balance resulting in steady weight decline.
Appetite suppression accompanies the metabolic changes, with many people experiencing reduced interest in food or early satiety during meals. Favorite foods may lose their appeal, and eating becomes more of a chore than pleasure. Nausea and abdominal discomfort can further complicate nutritional intake.
Children and elderly individuals show more dramatic weight loss patterns, often dropping below normal growth curves or losing significant percentages of body weight within months. These vulnerable populations require particularly vigilant monitoring for unexplained weight changes that could indicate tuberculosis infection.
3. Persistent fatigue and weakness
Chronic exhaustion represents another hallmark of early tuberculosis infection. This fatigue differs from normal tiredness after physical exertion or inadequate sleep. Instead, it presents as overwhelming weakness that fails to improve with rest and progressively worsens over weeks or months.
The immune system’s constant battle against tuberculosis bacteria depletes energy reserves normally available for daily activities. Inflammatory processes require substantial metabolic resources, leaving individuals feeling drained even after minimal physical or mental exertion. This fatigue often forces people to reduce work hours, social activities, or exercise routines.
Sleep disturbances compound the fatigue problem, with many tuberculosis patients experiencing night sweats, coughing episodes, or breathing difficulties that interrupt restorative sleep cycles. The combination of poor sleep quality and increased metabolic demands creates a cycle of worsening exhaustion.
Muscle weakness may accompany general fatigue, making routine tasks like climbing stairs, carrying groceries, or maintaining household responsibilities increasingly difficult. This physical decline often prompts family members to notice changes before the affected individual recognizes the severity of their condition.
4. Fever patterns and temperature fluctuations
Tuberculosis typically produces distinctive fever patterns that differ from acute infections like influenza or pneumonia. These temperature elevations often occur in the late afternoon or evening, returning to normal or near-normal levels by morning. This cyclical pattern can persist for weeks or months without resolution.
Low-grade fevers between 99-101°F characterize most tuberculosis cases, though some individuals experience higher temperatures during disease progression. The relatively modest temperature elevation leads many people to dismiss the fever as minor illness or stress-related symptoms.
Chills and sweating often accompany fever episodes, particularly during nighttime hours. These symptoms can disrupt sleep patterns and contribute to overall fatigue and weakness. Some people experience profuse sweating without recognizable fever, making temperature monitoring important for accurate assessment.
The intermittent nature of tuberculosis fever can create false reassurance when temperatures normalize temporarily. However, the recurring pattern over weeks distinguishes tuberculosis from self-limiting viral infections that typically resolve within days.
5. Night sweats and sleep disturbances
Profuse night sweating represents a classic tuberculosis symptom that can significantly impact sleep quality and daily functioning. These episodes involve drenching sweats that soak sleepwear and bedding, forcing frequent clothing and linen changes during the night.
The sweating typically occurs during deep sleep phases when fever peaks, awakening individuals in uncomfortable, wet conditions. This pattern can repeat multiple times per night, fragmenting sleep and preventing restorative rest cycles essential for immune function and recovery.
Unlike menopausal hot flashes or temporary sweating from room temperature, tuberculosis night sweats persist nightly for weeks or months. The consistency and severity distinguish these episodes from occasional sweating related to environmental factors or other medical conditions.
Sleep disruption from night sweats compounds other tuberculosis symptoms, worsening fatigue, reducing appetite, and impairing immune system function. The cyclical nature creates a downward spiral where poor sleep perpetuates disease progression and symptom severity.
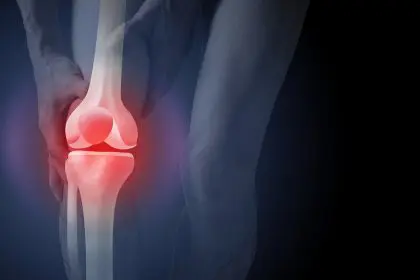
6. Chest pain and breathing difficulties
Respiratory discomfort manifests as sharp, stabbing chest pain that worsens with deep breathing, coughing, or physical movement. This pain typically localizes to specific areas of the chest where lung inflammation is most severe, though it can shift locations as the infection progresses.
Breathing difficulties begin subtly with mild shortness of breath during physical exertion. As tuberculosis advances, respiratory compromise becomes apparent during routine activities like walking upstairs, carrying objects, or even talking for extended periods. The progressive nature distinguishes tuberculosis from acute respiratory conditions.
Pleuritic pain occurs when tuberculosis infection spreads to the pleural lining surrounding the lungs. This sharp, knife-like pain intensifies dramatically with breathing movements, coughing, or position changes. The pain can be severe enough to limit normal activities and sleep positioning.
Some individuals develop a sensation of chest tightness or pressure rather than sharp pain. This feeling may be described as having a weight on the chest or difficulty expanding the lungs fully. The persistent nature and gradual worsening indicate serious underlying pathology requiring medical evaluation.
7. Changes in sputum production and appearance
Sputum characteristics provide crucial diagnostic information about tuberculosis progression and severity. Early infection may produce minimal sputum, but bacterial multiplication leads to increased production of thicker, more tenacious secretions that become difficult to clear from the respiratory system.
Color changes in sputum reflect disease progression and tissue damage within the lungs. Clear or white sputum gradually transitions to yellow or green as bacterial load increases and immune cells accumulate in respiratory secretions. Rust-colored or brown sputum indicates more advanced disease with tissue breakdown.
Blood streaking in sputum represents a significant development requiring immediate medical attention. Hemoptysis can range from occasional blood streaks to frank bleeding, indicating erosion of lung tissue or blood vessel damage from advanced tuberculosis infection.
Sputum consistency becomes increasingly thick and difficult to expectorate as tuberculosis progresses. Many people develop a sensation of thick secretions stuck in their throat or chest, requiring frequent attempts to clear their airways through coughing or throat clearing.
8. Loss of appetite and digestive changes
Appetite suppression occurs early in tuberculosis infection as bacterial toxins and inflammatory mediators interfere with normal hunger signals. Food loses its appeal, and many people find themselves eating mechanically rather than enjoying meals. This appetite loss contributes significantly to progressive weight reduction.
Nausea and early satiety compound feeding difficulties, with many individuals feeling full after consuming small portions. Favorite foods may trigger nausea or seem unpalatable, further limiting nutritional intake. These digestive changes can be mistaken for gastrointestinal disorders rather than systemic tuberculosis effects.
Abdominal discomfort and altered bowel patterns may accompany appetite changes. Some people experience cramping, bloating, or irregular bowel movements as tuberculosis affects multiple body systems. These digestive symptoms can mislead individuals and healthcare providers toward gastrointestinal diagnoses.
Nutritional deficiencies develop as reduced intake combines with increased metabolic demands from fighting infection. Vitamin and mineral deficiencies can exacerbate fatigue, immune dysfunction, and delayed healing, creating a cycle that perpetuates tuberculosis progression.
9. Swollen lymph nodes and immune system changes
Lymph node enlargement occurs as the immune system attempts to contain tuberculosis infection. These swollen nodes typically appear in the neck, armpits, or groin areas and may be tender to touch. The nodes can enlarge gradually over weeks or months rather than appearing suddenly like those associated with acute infections.
The lymphatic system’s response to tuberculosis creates palpable masses that persist despite typical treatments for swollen glands. These nodes may feel firm or rubbery and can become matted together as the infection progresses. Their persistent nature distinguishes tuberculosis-related lymphadenopathy from temporary swellings.
Immune system compromise becomes apparent through increased susceptibility to other infections, delayed wound healing, and general malaise. The body’s resources become focused on fighting tuberculosis, leaving reduced capacity to handle other health challenges or maintain normal immune surveillance.
Some individuals develop skin changes, including rashes or slow-healing wounds, reflecting overall immune system dysfunction. These manifestations may seem unrelated to respiratory symptoms but represent systemic effects of chronic tuberculosis infection.
Early recognition of these nine warning signs can make the difference between successful treatment and serious complications. Tuberculosis remains highly treatable when detected promptly, but delayed diagnosis allows progression to more severe forms that require longer treatment courses and carry higher complication risks. Anyone experiencing combinations of these symptoms, particularly persistent cough with weight loss and fatigue, should seek immediate medical evaluation for proper testing and diagnosis. Modern tuberculosis treatment offers excellent cure rates, but success depends on early intervention and complete treatment adherence.