Jaw pain affects millions of people daily, ranging from minor discomfort that resolves quickly to persistent aching that significantly impacts quality of life. While some jaw pain results from temporary muscle tension or minor irritation, certain patterns and characteristics indicate underlying dental problems that require professional evaluation and treatment.
The jaw joint, muscles, and surrounding structures work together in complex ways to enable chewing, speaking, and other essential functions. When dental problems develop, they often create pain patterns that extend beyond individual teeth to affect the entire jaw region. Understanding these connections helps distinguish between temporary discomfort and symptoms requiring dental intervention.
Recognizing when jaw pain signals dental problems empowers individuals to seek appropriate care before conditions worsen or cause permanent damage. Early identification of dental-related jaw pain can prevent complications, preserve oral health, and reduce the need for extensive treatments later.
1. Persistent throbbing pain that worsens with pressure
Dental infections often create deep, throbbing jaw pain that intensifies when pressure is applied to the affected area. This type of pain typically differs from muscle-related jaw discomfort by its persistent, pulsating quality that seems to originate from within the jawbone rather than surface muscles.
Infected tooth roots can cause severe jaw pain that radiates throughout the affected side of the face. The infection creates pressure within the tooth and surrounding bone structures, generating intense discomfort that often worsens when lying down or bending over due to increased blood flow to the area.
Abscessed teeth produce particularly severe jaw pain as bacterial infections create pockets of pus that press against surrounding tissues. This pressure creates constant discomfort that may be accompanied by swelling, fever, and a foul taste in the mouth indicating serious infection requiring immediate dental attention.
Deep cavities that have reached the tooth’s nerve center often cause referred pain throughout the jaw region. The infected or inflamed nerve tissue generates signals that the brain interprets as coming from various areas of the jaw, creating widespread discomfort that seems disproportionate to the visible tooth damage.
Cracked teeth can create intermittent but severe jaw pain, particularly when biting down or exposing the tooth to temperature changes. The crack allows bacteria to penetrate deeper tooth structures, creating infection and inflammation that manifests as jaw pain extending beyond the damaged tooth.
2. Pain triggered by temperature changes
Dental sensitivity that creates jaw pain in response to hot or cold foods and beverages often indicates significant tooth damage or decay. This temperature-related pain typically signals that tooth enamel has been compromised, allowing stimuli to reach sensitive inner tooth structures.
Exposed tooth roots due to gum recession can cause sharp, shooting pains that radiate throughout the jaw when consuming hot or cold items. The lack of protective enamel covering allows temperature changes to directly stimulate nerve endings, creating intense discomfort that extends beyond the affected tooth.
Deep cavities that have penetrated through enamel and dentin layers often create severe temperature sensitivity accompanied by jaw pain. The proximity of decay to the tooth’s nerve center means that temperature changes can trigger intense pain signals that spread throughout the jaw region.
Worn tooth enamel from grinding, acid erosion, or aggressive brushing can expose underlying dentin, creating sensitivity that manifests as jaw pain. This widespread enamel loss often affects multiple teeth simultaneously, creating generalized jaw discomfort in response to various triggers.
Cracked or fractured teeth allow temperature changes to reach internal tooth structures, creating sudden, sharp pains that radiate throughout the affected side of the jaw. These cracks may be invisible to casual observation but create significant sensitivity and discomfort.
3. Swelling and inflammation around the jaw
Visible swelling or inflammation in the jaw area often indicates serious dental infections that require immediate professional attention. This swelling typically represents the body’s immune response to bacterial infections originating from dental problems.
Facial swelling that begins near teeth and spreads to surrounding jaw tissues suggests dental abscesses that have extended beyond individual teeth. This type of swelling often feels firm or hard to the touch and may be accompanied by fever, indicating systemic involvement of the infection.
Gum swelling around specific teeth that extends to jaw tissues can indicate advanced periodontal disease or localized infections. The inflammation often creates pressure and discomfort throughout the jaw region while compromising the stability of affected teeth.
Lymph node swelling beneath the jaw often accompanies dental infections as the body’s immune system responds to bacterial invasion. These swollen nodes feel like tender lumps beneath the jawline and indicate that infection has spread beyond the localized dental area.
Internal mouth swelling that affects the floor of the mouth or inner cheek areas can indicate serious dental infections that threaten airway function. This type of swelling requires emergency dental care to prevent life-threatening complications.
4. Difficulty opening or closing the mouth
Restricted jaw movement that interferes with normal mouth opening or closing often indicates dental problems affecting jaw joint function or muscle coordination. This limitation typically develops gradually but can significantly impact eating, speaking, and oral hygiene.
Wisdom tooth problems frequently cause jaw stiffness and limited mouth opening as impacted teeth create pressure against surrounding structures. The inflammation and crowding associated with wisdom tooth issues can restrict normal jaw movement while creating significant discomfort.
Severe dental infections can cause muscle spasms and tissue swelling that limit jaw mobility. The body’s protective response to infection often includes muscle tightening designed to limit movement in affected areas, reducing normal jaw function.
Advanced periodontal disease can affect the ligaments and bones supporting teeth, creating jaw instability that interferes with normal movement patterns. This instability often manifests as difficulty coordinating jaw movements during chewing or speaking.
Dental trauma from accidents or injuries can damage jaw joints, muscles, or surrounding structures, creating movement restrictions that persist until proper treatment addresses the underlying damage.
5. Pain that intensifies during chewing
Jaw pain that specifically worsens during chewing or biting often indicates dental problems affecting individual teeth or their supporting structures. This functional pain differs from general jaw discomfort by its direct relationship to dental activities.
Loose teeth from advanced periodontal disease create pain during chewing as damaged support structures cannot adequately stabilize teeth during normal function. The movement of loose teeth during chewing creates pressure and discomfort throughout the jaw region.
Cracked or fractured teeth often cause sharp, intense pain during biting that radiates throughout the jaw. The pressure of chewing forces crack segments apart, stimulating exposed nerve tissues and creating widespread discomfort.
Poorly fitting dental restorations like crowns or fillings can create uneven bite pressures that cause jaw pain during chewing. These restoration problems often develop gradually as dental work settles or wears, creating new pressure points that stress jaw muscles and joints.
Missing teeth can create uneven chewing patterns that overload remaining teeth and stress jaw muscles. The compensation required to chew effectively with missing teeth often leads to muscle fatigue and joint stress that manifests as widespread jaw pain.
6. Nighttime pain that disrupts sleep
Jaw pain that specifically occurs at night or disrupts sleep patterns often indicates dental problems that worsen during periods of unconscious teeth grinding or clenching. This nocturnal pain typically results from increased pressure on already compromised dental structures.
Tooth grinding during sleep can exacerbate existing dental problems, creating intense jaw pain that awakens individuals from sleep. The sustained pressure and friction of grinding can inflame already damaged teeth, nerves, or supporting structures.
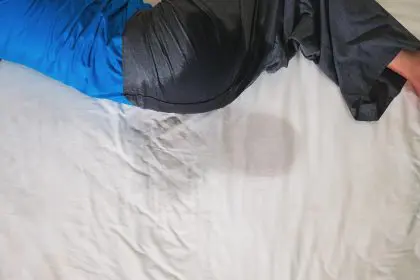
Infected teeth often create throbbing pain that intensifies when lying down due to increased blood flow to the head region during horizontal positioning. This positional component of dental pain often makes sleep difficult and indicates serious infection requiring treatment.
Advanced cavities that have reached tooth nerve centers often create spontaneous pain that occurs without obvious triggers, frequently disrupting sleep patterns. This unprovoked pain typically indicates irreversible nerve damage requiring immediate dental intervention.
Dental abscesses can create constant, severe pain that prevents restful sleep as bacterial infections generate continuous pressure and inflammation within jaw tissues. This persistent pain often worsens at night when other distractions are minimal.
7. Accompanied by changes in bite alignment
Jaw pain accompanied by noticeable changes in how teeth fit together often indicates significant dental problems affecting tooth position or jaw joint function. These bite changes typically develop gradually but can create cascading problems throughout the oral system.
Tooth loss from decay, trauma, or periodontal disease can cause remaining teeth to shift position, creating bite imbalances that stress jaw joints and muscles. The compensation required to achieve proper tooth contact often creates jaw pain and dysfunction.
Advanced periodontal disease can cause teeth to become loose and shift position, altering bite relationships and creating uneven pressure distribution during chewing. This bite instability often results in jaw muscle fatigue and joint stress.
Worn teeth from grinding, acid erosion, or normal aging can change bite height and tooth relationships, forcing jaw joints to function in altered positions that create pain and dysfunction over time.
Dental restorations that are too high or poorly contoured can create premature tooth contacts that force jaw joints into strained positions during closing. These high spots often create localized pressure points that generate widespread jaw discomfort.
8. Associated with bad breath or unusual tastes
Jaw pain accompanied by persistent bad breath or unusual tastes in the mouth often indicates dental infections that require immediate professional attention. These additional symptoms suggest bacterial involvement that extends beyond localized tooth problems.
Periodontal disease creates deep pockets between teeth and gums where bacteria accumulate, producing foul odors and tastes while contributing to jaw pain through chronic inflammation. The persistent bacterial presence often creates ongoing discomfort that affects jaw function.
Dental abscesses produce characteristic foul tastes and odors as infected tissue breaks down and bacterial toxins accumulate. The drainage from these infections often creates metallic or bitter tastes while generating significant jaw pain from internal pressure.
Food trapped in cavities or between damaged teeth can decay and produce offensive odors while contributing to ongoing infection and inflammation. The bacterial growth in these areas often extends to surrounding tissues, creating jaw pain and systemic symptoms.
Infected wisdom teeth often create particularly strong odors and tastes as bacteria accumulate in areas that are difficult to clean effectively. The combination of infection and limited access for cleaning often results in severe jaw pain and noticeable oral symptoms.
Recognition of these warning signs enables timely intervention that can prevent dental problems from progressing to more serious complications. Jaw pain that exhibits these characteristics typically indicates conditions requiring professional dental evaluation and treatment rather than simple home management.
The complex relationship between dental health and jaw function means that seemingly minor dental problems can create significant jaw pain and dysfunction. Understanding these connections helps individuals recognize when professional care is necessary for proper diagnosis and treatment.
Early intervention for dental-related jaw pain often prevents the need for more extensive and expensive treatments while preserving oral health and function. Ignoring these warning signs can lead to tooth loss, chronic pain, and complications that significantly impact quality of life.
Modern dentistry offers numerous effective treatments for dental problems causing jaw pain, ranging from simple procedures to complex reconstructive work. The key to successful treatment lies in recognizing symptoms early and seeking appropriate professional care before conditions progress to irreversible stages.
Maintaining regular dental checkups and good oral hygiene practices helps prevent many of the dental problems that cause jaw pain. However, when warning signs develop, prompt professional evaluation ensures the best possible outcomes for both dental health and jaw function.