Digestive discomfort affects nearly everyone at some point, but persistent symptoms can signal two very different conditions that millions of people struggle to distinguish. Irritable bowel syndrome and colon cancer both target the large intestine, creating overlapping symptoms that can cause confusion, delayed diagnosis, and unnecessary anxiety for those experiencing digestive troubles.
The distinction between these conditions extends far beyond simple symptom comparison, involving fundamental differences in causes, progression patterns, and treatment approaches. Understanding these differences empowers individuals to recognize when digestive symptoms warrant immediate medical attention versus lifestyle modifications and symptom management strategies.
Both conditions significantly impact quality of life, but their trajectories and outcomes differ dramatically. While one represents a chronic functional disorder that can be managed effectively, the other constitutes a serious malignancy requiring prompt intervention. Recognizing the subtle yet crucial differences between these conditions can literally save lives.
Understanding irritable bowel syndrome fundamentals
Irritable bowel syndrome represents a functional gastrointestinal disorder affecting the communication pathways between the brain and digestive system. This breakdown in neural signaling creates erratic bowel patterns, abdominal discomfort, and digestive unpredictability that characterizes the condition. The disorder affects approximately one in seven adults, making it among the most common digestive complaints.
The condition operates through disrupted gut-brain communication rather than structural abnormalities within the intestinal tract. This functional nature means that while symptoms can be severely disruptive, the actual tissue remains healthy and undamaged. The absence of tissue damage distinguishes IBS from inflammatory bowel diseases and malignant conditions that cause physical changes to intestinal structures.
Symptom patterns in IBS typically fluctuate based on various triggers including stress levels, dietary choices, hormonal changes, and sleep quality. These fluctuations create periods of relative comfort alternating with symptom flares, establishing the intermittent pattern that characterizes the condition. This variability often complicates diagnosis and treatment planning.
The nature of colon cancer development
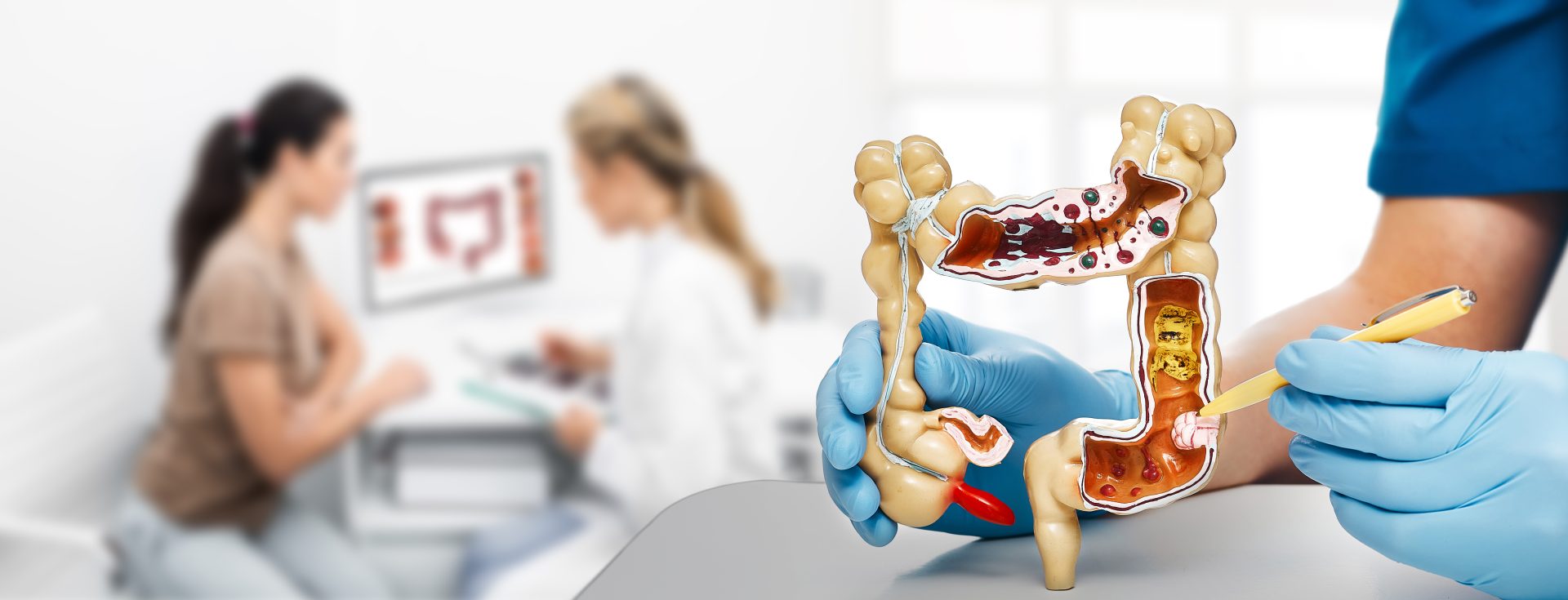
Colon cancer develops when normal cells within the large intestine undergo genetic mutations that cause uncontrolled growth and division. These cellular changes typically begin as small, benign growths called polyps that can gradually transform into malignant tumors over several years. The transformation process usually occurs slowly, providing opportunities for early detection through screening programs.
Unlike functional disorders, colon cancer creates actual physical changes within intestinal tissue that can be observed through imaging and direct visualization techniques. These structural alterations progress steadily without the fluctuating patterns seen in functional conditions. The progressive nature means symptoms typically worsen over time rather than improving spontaneously.
The malignant nature of colon cancer means affected cells can spread beyond the original tumor site, potentially affecting other organs and body systems. This metastatic potential distinguishes cancer from benign conditions and creates urgency around early detection and treatment. The ability to spread makes colon cancer a systemic threat rather than a localized digestive issue.
Overlapping symptoms that create confusion
- Abdominal pain and cramping occur in both conditions but follow different patterns. IBS-related pain often correlates with bowel movements and may improve after evacuation, while cancer-related pain tends to be more persistent and progressive. The pain location can also differ, with IBS typically causing lower abdominal discomfort and cancer potentially affecting various abdominal regions.
- Changes in bowel habits manifest differently between the conditions. IBS creates alternating patterns of diarrhea and constipation that may fluctuate within days or weeks, while colon cancer typically causes more consistent changes that worsen gradually. The stool characteristics also differ, with IBS rarely producing blood while colon cancer may cause visible or microscopic bleeding.
- Bloating and gas frequently accompany both conditions but respond differently to interventions. IBS-related bloating often improves with dietary modifications and stress management, while cancer-related bloating may persist despite lifestyle changes. The timing of bloating symptoms can also provide clues about underlying causes.
Distinctive warning signs of each condition
Colon cancer produces several symptoms rarely associated with IBS, creating important diagnostic clues for healthcare providers and patients. Unexplained weight loss represents a significant red flag that suggests malignancy rather than functional digestive issues. This weight loss occurs despite normal or increased appetite and cannot be attributed to intentional dietary changes.
Persistent rectal bleeding or blood in stool indicates potential tissue damage that doesn’t occur with IBS. While hemorrhoids and other benign conditions can cause bleeding, new or changing bleeding patterns warrant investigation to rule out malignancy. The appearance of blood can provide additional diagnostic information about potential causes.
Severe fatigue and weakness may accompany colon cancer due to internal bleeding that causes anemia. This fatigue differs from the general tiredness that can accompany IBS flares, typically being more persistent and severe. Iron deficiency anemia from chronic blood loss creates distinctive symptoms that healthcare providers can identify through blood testing.
Risk factors and prevention strategies
IBS risk factors include psychological stress, certain dietary patterns, hormonal fluctuations, and previous gastrointestinal infections. Managing these risk factors through stress reduction techniques, dietary modifications, and lifestyle improvements can significantly reduce symptom frequency and severity. The functional nature of IBS means that addressing triggers often provides substantial relief.
Colon cancer risk factors encompass age, family history, inflammatory bowel diseases, certain genetic syndromes, and lifestyle factors including diet and physical activity levels. While some risk factors cannot be modified, others respond well to lifestyle interventions that may reduce cancer development risk. Understanding personal risk profiles helps guide screening recommendations and prevention strategies.
Dietary approaches differ significantly between the conditions. IBS management often involves identifying and avoiding trigger foods, with low-FODMAP diets showing particular effectiveness for many individuals. Colon cancer prevention focuses on increasing fiber intake, reducing processed meat consumption, and maintaining overall dietary quality with abundant fruits and vegetables.
Diagnostic approaches and screening methods
IBS diagnosis relies primarily on symptom patterns and the exclusion of other conditions rather than specific diagnostic tests. Healthcare providers use established criteria that consider symptom duration, characteristics, and associated features to make accurate diagnoses. The process often involves ruling out inflammatory conditions, infections, and malignancies that can mimic IBS symptoms.
Colon cancer screening utilizes direct visualization techniques including colonoscopy, which allows healthcare providers to examine the entire colon lining for abnormalities. This screening approach can detect precancerous polyps before they transform into malignant tumors, providing opportunities for prevention rather than just early detection. Alternative screening methods include stool-based tests that detect blood or abnormal DNA.
Age considerations play crucial roles in diagnostic approaches, with colon cancer screening typically beginning at age 45 for average-risk individuals. However, concerning symptoms warrant investigation regardless of age, particularly when red flag symptoms suggest possible malignancy. Family history and other risk factors may indicate earlier or more frequent screening needs.
Treatment philosophies and approaches
IBS treatment focuses on symptom management and quality of life improvement rather than curing an underlying disease process. This approach emphasizes dietary modifications, stress management techniques, medications for specific symptoms, and psychological support when needed. The goal involves finding sustainable strategies that minimize symptom impact on daily activities.
Dietary interventions for IBS often begin with identifying trigger foods and implementing elimination protocols to determine individual sensitivities. Fiber modifications, probiotic supplementation, and specific dietary patterns like low-FODMAP approaches can provide significant symptom relief for many individuals. The personalized nature of dietary triggers means treatment plans must be individualized.
Colon cancer treatment aims to eliminate malignant cells and prevent disease spread through aggressive interventions including surgery, chemotherapy, and radiation therapy. Treatment intensity corresponds to cancer stage and spread, with early-stage cancers often curable through surgical removal alone. Advanced stages require multimodal approaches combining several treatment methods.
Psychological impact and mental health considerations
Both conditions significantly affect mental health, though through different mechanisms. IBS creates chronic uncertainty about symptom patterns that can lead to anticipatory anxiety and social isolation due to unpredictable digestive episodes. The chronic nature of symptoms can contribute to depression and reduced quality of life over time.
Colon cancer diagnosis creates acute psychological distress related to mortality concerns, treatment side effects, and lifestyle disruptions. The cancer journey involves multiple stressors including treatment decisions, financial concerns, and family impact that extend beyond physical symptoms. Support systems become crucial for managing these psychological challenges.
Stress management becomes important for both conditions but serves different purposes. IBS management benefits from stress reduction because psychological stress directly triggers symptom flares through gut-brain communication pathways. Cancer patients benefit from stress management primarily for overall well-being and treatment tolerance rather than direct symptom control.
When to seek immediate medical attention
Certain symptoms require prompt medical evaluation regardless of suspected underlying cause. Severe abdominal pain that interferes with daily activities or sleep warrants immediate assessment, particularly when accompanied by fever, vomiting, or signs of dehydration. These symptoms may indicate complications requiring urgent intervention.
Blood in stool, whether visible or detected through testing, always requires medical evaluation to determine the source and appropriate treatment. While many causes are benign, the possibility of malignancy necessitates prompt investigation. Changes in bleeding patterns or new bleeding episodes warrant particular attention.
Unintentional weight loss exceeding 10 pounds over several months suggests possible underlying malignancy and requires comprehensive evaluation. This symptom rarely accompanies functional digestive disorders and should prompt consideration of more serious conditions. Associated symptoms may provide additional clues about underlying causes.
Long-term outlook and prognosis
IBS represents a chronic condition that requires ongoing management but doesn’t increase mortality risk or predispose to serious complications. Most individuals learn to manage symptoms effectively through lifestyle modifications and appropriate treatments, maintaining good quality of life despite occasional symptom flares. The condition doesn’t typically worsen significantly over time.
Colon cancer prognosis depends heavily on stage at diagnosis, with early-stage cancers often completely curable through appropriate treatment. Five-year survival rates exceed 90% for localized cancers but decrease significantly when cancer has spread to distant organs. Early detection through screening programs dramatically improves outcomes.
The importance of distinguishing between these conditions cannot be overstated, as appropriate recognition leads to proper treatment and optimal outcomes for both conditions. Understanding the differences empowers individuals to seek appropriate care and advocate effectively for their health needs.