You tell yourself it’s just one week. Maybe you’re swamped at work, dealing with a family crisis, or nursing a minor injury that gives you the perfect excuse to skip your usual workout routine. Seven measly days off from exercise – what could possibly go wrong in such a short time?
Your arteries, apparently, have very strong opinions about your temporary retirement from physical activity. While you’re enjoying the freedom from sweaty gym clothes and early morning alarm clocks, your cardiovascular system is staging a silent rebellion that starts within hours of your last workout.
It turns out that your circulatory system is like a high-maintenance relationship that falls apart the moment you stop putting in effort. Those blood vessels that seemed so forgiving when you were exercising regularly become surprisingly vindictive when you abandon them for Netflix and takeout.
The scary part isn’t what happens after months or years of inactivity – it’s how quickly your arterial health starts deteriorating the moment you decide to take a “short break” from exercise.
Your blood vessels forget their training within days
Think of your arteries as elite athletes who’ve been training for peak performance. When you exercise regularly, these blood vessels become incredibly efficient at expanding and contracting, adjusting blood flow, and maintaining optimal pressure throughout your circulatory system.
But just like athletes lose conditioning when they stop training, your arteries begin losing their flexibility and responsiveness almost immediately when you become sedentary. Within 48 to 72 hours of skipping exercise, the smooth muscle cells that line your arteries start becoming stiffer and less reactive.
This isn’t just a gradual decline that you might not notice – it’s a measurable decrease in what scientists call endothelial function, which is basically your arteries’ ability to do their job properly. Your blood vessels literally forget how to respond appropriately to changes in blood flow and pressure.
The endothelium, which is the thin layer of cells lining your arteries, relies on the mechanical stimulation from increased blood flow during exercise to stay healthy and responsive. Remove that stimulus, and these cells start behaving like they’re retired from active duty.
Blood flow patterns shift into emergency mode
When you’re physically active, your heart pumps blood more forcefully and your arteries have to adapt quickly to handle varying demands. This creates a beneficial stress response that keeps your entire circulatory system flexible and efficient.
Stop exercising, and your cardiovascular system shifts into what can only be described as conservation mode. Blood flow becomes sluggish and predictable, like a river that’s stopped flowing fast enough to stay clear and starts developing stagnant pools.
Your heart doesn’t have to work as hard when you’re sedentary, which sounds good until you realize that cardiac muscle, like any other muscle, begins to weaken when it’s not challenged regularly. Within a week, your resting heart rate starts creeping upward as your heart becomes less efficient at pumping blood.
The reduced blood flow also affects how well your arteries can deliver oxygen and nutrients to tissues throughout your body. Areas that depend on good circulation, like your brain and extremities, begin receiving less optimal blood supply even though you might not notice any obvious symptoms yet.
Inflammation markers spike like a fever
Exercise acts as a natural anti-inflammatory medication for your cardiovascular system, helping to keep arterial walls smooth and healthy. When you stop moving, inflammatory processes that were being suppressed by regular physical activity suddenly have free rein to cause trouble.
Within days of becoming sedentary, blood markers of inflammation begin rising throughout your circulatory system. It’s like your immune system suddenly decides that your arteries are suspicious and need to be attacked, creating exactly the kind of chronic inflammation that leads to cardiovascular disease.
C-reactive protein, interleukin-6, and other inflammatory compounds start accumulating in your bloodstream and arterial walls. These substances make your arteries more prone to developing the kind of damage that eventually leads to atherosclerosis, blood clots, and heart attacks.
The inflammatory response also makes your arteries more reactive to stress hormones like cortisol and adrenaline. This means that everyday stressors that wouldn’t have fazed your cardiovascular system during your active period now cause more dramatic spikes in blood pressure and heart rate.
Blood pressure regulation goes haywire
Your arteries are constantly making tiny adjustments to maintain optimal blood pressure as you move through different activities and positions throughout the day. Regular exercise trains this regulatory system to be incredibly precise and responsive.
Skip exercise for a week, and this fine-tuned blood pressure control system starts malfunctioning like a thermostat with a broken sensor. Your arteries become less capable of making the rapid adjustments needed to maintain steady pressure when you stand up, climb stairs, or experience emotional stress.
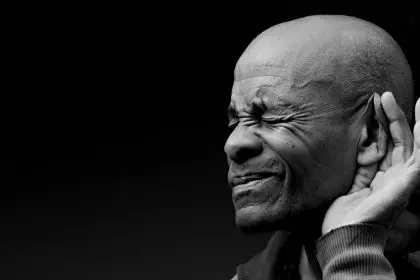
Many people notice that they feel slightly dizzy or lightheaded when standing up quickly after being sedentary for several days. This isn’t just from being out of shape – it’s a sign that your arterial system is losing its ability to quickly redirect blood flow where it’s needed.
Blood pressure variability also increases during periods of inactivity. Instead of maintaining relatively stable pressure throughout the day, you might experience more dramatic swings between high and low readings as your arterial control mechanisms become less reliable.
Arterial stiffness increases like aging in fast forward
One of the most concerning changes that happens during exercise breaks is how quickly your arteries begin to stiffen. Arterial flexibility is crucial for healthy circulation and blood pressure regulation, and it’s one of the first things to deteriorate when you become inactive.
This stiffening process normally happens gradually with aging, but lack of exercise accelerates it dramatically. Within a week of inactivity, your arteries begin behaving like they belong to someone significantly older than you actually are.
Pulse wave velocity, which measures how fast pressure waves travel through your arteries, increases when you’re sedentary. Faster pulse wave velocity indicates stiffer arteries that can’t absorb and release pressure waves effectively, leading to higher blood pressure and increased stress on your heart.
The stiffening also affects your arteries’ ability to expand during periods of increased blood flow demand. This means that when you do try to return to physical activity, your cardiovascular system will struggle more than usual to meet the increased oxygen and nutrient demands.
Metabolic changes sabotage arterial health
Exercise doesn’t just benefit your arteries directly – it also improves the metabolic environment that your blood vessels have to operate in. When you stop exercising, metabolic changes occur that make it harder for your arteries to stay healthy.
Insulin sensitivity decreases within days of becoming sedentary, leading to higher blood sugar levels that can damage arterial walls. Your body also becomes less efficient at using fats for energy, leading to changes in blood lipid profiles that promote arterial inflammation and plaque formation.
Blood sugar spikes become more dramatic and last longer when you’re inactive, exposing your arterial walls to periods of high glucose that can cause oxidative damage. This is particularly problematic if you continue eating the same way you did when you were exercising regularly.
The metabolic slowdown also affects how your body processes stress hormones, inflammatory compounds, and other substances that can harm arterial health. Your liver, muscles, and other tissues become less efficient at clearing these potentially harmful substances from your bloodstream.
Recovery takes longer than you expect
The depressing reality is that while arterial damage from a week of inactivity happens quickly, restoring optimal function takes considerably longer. Your cardiovascular system doesn’t just snap back to its previous condition the moment you lace up your sneakers again.
Endothelial function, arterial flexibility, and blood pressure regulation all need time to return to their pre-break levels. Depending on your baseline fitness and how sedentary you were during your exercise hiatus, full recovery might take two to four weeks of consistent activity.
This recovery period is why many people feel unusually winded or experience higher heart rates when they return to exercise after even short breaks. Your arteries are essentially starting from a deficit and need time to remember how to support physical activity efficiently.
The good news is that younger, healthier arteries recover faster than older or damaged ones. But the lesson is clear – your cardiovascular system thrives on consistency and doesn’t handle exercise vacations as gracefully as you might hope.
Prevention beats damage control every time
Understanding how quickly arterial health deteriorates during exercise breaks should motivate you to find ways to stay active even during busy or challenging periods. You don’t need to maintain your full workout routine, but some movement is infinitely better than complete inactivity.
Even light walking, stretching, or basic bodyweight exercises can help maintain arterial function during periods when your normal routine isn’t possible. The key is keeping blood flowing and giving your cardiovascular system some level of challenge to work with.
Your arteries are remarkably responsive to physical activity – they can improve quickly when you’re consistent, but they can also deteriorate rapidly when neglected. Treating exercise as non-negotiable rather than optional might be the best investment you can make in your long-term cardiovascular health.