Stress is often seen as a mental and emotional burden, but its effects reach far deeper than most realize. For many, chronic stress doesn’t just weigh on the mind — it can amplify physical pain in ways that are both subtle and severe. Understanding how stress intensifies pain in the body is not just enlightening — it’s critical to reclaiming comfort, energy and emotional well-being.
The connection between stress and physical pain
The body is a finely tuned system. When you experience stress, it reacts with a flood of hormones like cortisol and adrenaline. These hormones trigger the “fight-or-flight” response, originally designed to protect us from immediate danger. But in modern life, where stress can be constant and unresolved, this reaction becomes harmful.
Persistent stress keeps your body in a heightened state of alert. Over time, this tension overstimulates the nervous system and increases sensitivity to pain. For individuals already coping with chronic pain conditions — such as arthritis, migraines, fibromyalgia or back problems — stress can make their symptoms worse.
Why muscles tense up under pressure
One of the first ways stress affects the body is by tightening muscles. This is the body’s attempt to shield you from perceived danger. It’s an ancient survival tactic. But when stress never lets up, neither do your muscles.
Tense muscles lead to joint stiffness, increased soreness and reduced mobility. Think of the tightness in your shoulders or the aching in your lower back after a long day. These aren’t random discomforts. They’re physical echoes of unrelieved stress.
This tension doesn’t just come and go. It builds — gradually locking the body into painful patterns. The pain may start in one area but can radiate to others, creating an overwhelming sensation that seems impossible to control.
How stress alters brain pain perception
Stress doesn’t just make pain feel worse — it actually rewires how your brain responds to it.
The brain’s pain-processing regions, such as the amygdala and the anterior cingulate cortex, become hyperactive when you’re under emotional strain. This means that even mild discomfort can feel unbearable when you’re stressed.
Furthermore, chronic stress reduces the brain’s production of serotonin and dopamine — neurotransmitters responsible for mood regulation and natural pain relief. A decrease in these chemicals makes pain feel more intense and your coping ability weaker.
It’s a double blow: more pain and less resilience to manage it.
The vicious cycle of stress and pain
The relationship between stress and pain can become a vicious loop. Pain increases stress, and stress increases pain. This cycle can trap individuals in a state of physical and emotional exhaustion.
For example, someone with a history of neck pain may feel more discomfort when going through financial hardship or a relationship crisis. That pain, in turn, makes sleep more difficult, reduces focus and limits daily activity — all of which create even more stress.
Breaking this loop is essential for healing, but it requires recognizing the link between emotional strain and physical symptoms.
Conditions most affected by stress-induced pain
While everyone experiences stress differently, certain conditions are more vulnerable to its effects:
- Tension headaches: Often caused by tightened muscles in the neck, jaw or shoulders
- Irritable bowel syndrome (IBS): Stress disrupts gut-brain communication, leading to cramping, bloating and discomfort
- Back pain: Stress-related posture changes and muscle strain intensify lower and upper back pain
- Fibromyalgia: Stress heightens the sensitivity of pain receptors, worsening widespread pain
- TMJ (Temporomandibular Joint) disorders: Clenching or grinding teeth during stressful periods causes jaw pain and headaches
Understanding these conditions and their triggers is a step toward relief.
Managing stress to ease physical pain
Fortunately, the connection between stress and pain offers a path forward. By managing stress, many individuals report significant improvements in their physical symptoms. Here are some proven strategies:
Mindful breathing and meditation: These calm the nervous system and reduce muscle tension.
Exercise: Regular movement releases endorphins — natural painkillers that elevate mood and ease discomfort.
Therapy or counseling: Emotional release can ease physical burdens. Speaking with a mental health professional helps break long-standing stress patterns.
Sleep hygiene: A rested body is more resilient. Aim for consistency and comfort in your sleep environment.
Social support: Connecting with others reduces the feeling of isolation, which can fuel stress and pain.
These aren’t luxury solutions — they’re vital steps for reclaiming your quality of life.
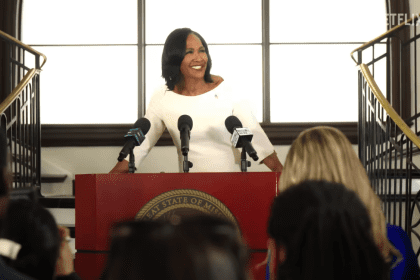
The role of medical professionals
Doctors, physical therapists and mental health providers are increasingly aware of how emotional stress manifests as physical discomfort. If pain persists and doesn’t respond to conventional treatment, it may be time to look deeper.
Pain management today often includes a multidisciplinary approach, addressing both the body and the mind. Cognitive-behavioral therapy, mindfulness-based stress reduction and guided relaxation are all tools being used alongside medication or physical therapy.
This holistic approach reflects a new understanding: healing must involve the whole person — not just isolated symptoms.
Choosing restoration over reaction
In a world where hustle is glorified and downtime is rare, it’s no surprise that many live with pain they don’t fully understand. But when we recognize how stress intensifies pain in the body, we take the first step toward healing.
You don’t have to live in constant discomfort. Identifying stress as a cause — not just a side effect — of physical pain is an empowering realization. With compassion, strategy and support, it’s possible to reduce both emotional strain and the physical pain it feeds.
It begins with listening — not just to your thoughts, but to the quiet messages your body has been sending all along.