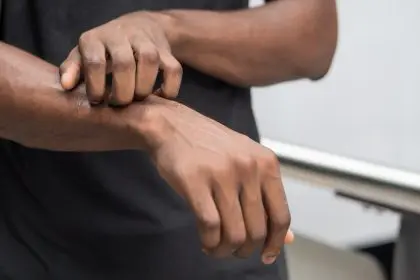
A peculiar skin transformation is affecting millions of people worldwide, turning the outermost layer of healthy skin into a sponge-like structure that triggers relentless itching, mysterious rashes, and fluid-filled blisters that can dramatically alter daily life. Spongiotic dermatitis represents one of the most misunderstood and underdiagnosed skin conditions, often dismissed as simple eczema when it actually involves complex inflammatory processes that can lead to serious complications if left untreated.
This condition operates through mechanisms that most people never learn about, creating skin changes that extend far beyond surface-level irritation to affect the fundamental structure of the epidermis itself. The transformation occurs at a cellular level, where inflammation disrupts normal skin barriers and creates the characteristic spongy appearance that gives the condition its distinctive name.
Understanding spongiotic dermatitis requires recognizing that it represents not just one condition but rather a pattern of skin response that can develop from multiple underlying causes, each requiring different treatment approaches and management strategies. The complexity of this condition explains why so many people struggle with recurring symptoms despite trying numerous treatments that address only surface-level manifestations.
Cellular transformation creates sponge-like skin texture
The first remarkable aspect of spongiotic dermatitis lies in its ability to fundamentally alter the cellular structure of the epidermis, creating intercellular fluid accumulation that gives affected skin its characteristic spongy appearance under microscopic examination. This transformation occurs when inflammatory processes disrupt the normal connections between skin cells, allowing fluid to accumulate in spaces that should remain tightly sealed.
The spongiotic process begins with immune system activation that triggers inflammatory mediators to flood the epidermis, causing skin cells to separate and create microscopic gaps filled with inflammatory fluid. This cellular separation explains why affected skin often appears swollen, feels tender to touch, and develops the scaling patterns that characterize various forms of the condition.
The extent of spongiotic changes varies significantly between individuals and can fluctuate over time, with some people experiencing mild cellular separation that creates subtle texture changes while others develop severe spongiosis that leads to blister formation and significant skin barrier compromise. These variations help explain why the condition presents so differently across affected populations.
The cellular transformation process is reversible in early stages but can become permanent if inflammation persists chronically, leading to structural changes that affect skin function long-term. Understanding this progression helps explain why early intervention proves so crucial for preventing lasting skin damage.
Multiple underlying conditions trigger identical symptoms
The second surprising characteristic of spongiotic dermatitis involves its development from numerous different underlying conditions that all produce similar spongiotic changes in the epidermis, making accurate diagnosis challenging without comprehensive evaluation. Atopic dermatitis, contact dermatitis, dyshidrotic eczema, nummular eczema, and seborrheic dermatitis can all manifest with identical spongiotic patterns despite having completely different root causes.
Atopic dermatitis creates spongiotic changes through genetic predisposition and immune system dysfunction that makes skin hyperreactive to environmental triggers, while contact dermatitis develops spongiosis through direct chemical irritation or allergic responses to specific substances. These different mechanisms require entirely different treatment approaches despite producing similar skin appearances.
Dyshidrotic eczema generates spongiotic changes specifically on hands and feet through unclear mechanisms that may involve stress, metal allergies, or seasonal factors, while nummular eczema creates distinctive coin-shaped spongiotic patches that often develop after skin injuries or during dry weather conditions.
Seborrheic dermatitis produces spongiotic changes through yeast overgrowth and oil gland dysfunction, particularly affecting scalp and facial areas where sebaceous glands are most concentrated. This variety of underlying causes explains why treatment approaches that work for one person may prove completely ineffective for another with identical-appearing symptoms.
Hidden risk factors increase susceptibility dramatically
The third crucial understanding involves recognizing that spongiotic dermatitis susceptibility is influenced by numerous hidden risk factors that many people never associate with skin problems, including immune system status, occupational exposures, family genetics, and even age-related changes in skin barrier function.
Immune system dysfunction significantly increases spongiotic dermatitis risk, with people who have weakened immunity from illness, medications, or chronic stress showing much higher rates of skin inflammation and slower healing responses. This connection explains why the condition often worsens during periods of illness or high stress when immune resources are depleted.
Occupational exposures create cumulative damage that increases spongiotic dermatitis susceptibility over time, with healthcare workers, cleaning professionals, mechanics, and others who regularly contact irritating substances showing elevated rates of the condition. Even seemingly mild exposures can trigger spongiotic changes in susceptible individuals.
Family history plays a significant role in spongiotic dermatitis development, with genetic factors affecting skin barrier function, immune responses, and inflammatory tendencies that predispose certain individuals to developing the condition. Understanding family patterns helps predict risk and guide prevention strategies.
Age-related changes in skin structure and function create windows of increased vulnerability, with infants having underdeveloped skin barriers and elderly individuals experiencing decreased skin repair capacity that makes them more susceptible to spongiotic changes from environmental triggers.
Symptom patterns reveal condition severity and prognosis
The fourth important insight involves understanding how symptom patterns and progression provide crucial information about condition severity, underlying causes, and likely treatment responses that can guide more effective management approaches. The specific combination of symptoms often reveals more about the condition than any single manifestation.
Intense itching that worsens at night typically indicates more severe spongiotic changes and suggests the need for aggressive anti-inflammatory treatment, while mild itching that responds to moisturizing may indicate early-stage condition that can be managed with topical care alone. The timing and triggers of itching episodes provide valuable diagnostic clues.
Fluid-filled blisters that develop spontaneously suggest severe spongiotic changes that require immediate medical attention, while dry scaling without blistering may indicate chronic low-grade inflammation that responds well to barrier repair treatments. The presence of fluid leakage often indicates secondary bacterial infection that complicates treatment.
Coin-shaped patches suggest nummular eczema patterns, while hand and foot involvement points toward dyshidrotic variants that require specialized treatment approaches. The distribution pattern of symptoms helps identify underlying triggers and guide targeted interventions.
Color changes in affected skin provide important prognostic information, with bright red inflammation suggesting acute flares that respond well to treatment, while darkened, thickened skin indicates chronic changes that may require long-term management strategies to prevent permanent damage.
Treatment approaches require personalized strategies
The fifth critical aspect involves recognizing that effective spongiotic dermatitis treatment requires highly personalized approaches that address individual trigger patterns, symptom severity, lifestyle factors, and underlying health conditions rather than applying generic treatment protocols that may prove ineffective or even harmful.
Topical steroid treatments work effectively for inflammatory flares but require careful selection of potency levels and application schedules based on skin thickness, symptom severity, and individual response patterns. Using inappropriate steroid strengths can cause skin thinning or rebound flares that worsen the underlying condition.
Moisturizing strategies must be tailored to individual skin types and environmental conditions, with some people requiring heavy occlusive moisturizers while others benefit from lighter formulations that don’t trigger additional irritation. The timing of moisturizer application significantly affects effectiveness.
Dietary modifications can dramatically improve symptoms in some individuals, particularly those with food allergies or sensitivities that trigger inflammatory responses, while other people show no dietary connections and may waste time pursuing ineffective nutritional interventions instead of addressing actual triggers.
Stress management becomes crucial for people whose spongiotic dermatitis flares during periods of emotional or physical stress, while others show no stress connections and benefit more from environmental trigger avoidance or barrier protection strategies.
Complications develop without proper management
The sixth alarming reality involves understanding that untreated or poorly managed spongiotic dermatitis can lead to serious complications that extend far beyond cosmetic concerns to include infections, permanent skin changes, and psychological impacts that affect overall quality of life and wellbeing.
Secondary bacterial infections develop when compromised skin barriers allow harmful microorganisms to penetrate deeper skin layers, creating painful, pus-filled lesions that require antibiotic treatment and can leave permanent scarring. These infections can spread rapidly and may require hospitalization in severe cases.
Chronic scratching leads to lichenification, a permanent thickening and darkening of skin that creates leathery texture changes that persist even after inflammation resolves. This complication significantly affects appearance and can cause ongoing discomfort and reduced skin flexibility.
Sleep disruption from intense nighttime itching creates cascading health effects including impaired immune function, increased stress hormone levels, and reduced healing capacity that perpetuates the inflammatory cycle. Chronic sleep loss affects work performance, relationships, and mental health.
Social isolation often develops as people become self-conscious about visible skin changes, avoiding activities and relationships that previously brought joy and fulfillment. This psychological impact can lead to depression and anxiety that require professional mental health support.
Prevention strategies offer hope for long-term control
The seventh empowering insight involves understanding that comprehensive prevention strategies can significantly reduce spongiotic dermatitis flare frequency and severity, allowing many people to achieve long-term symptom control without relying solely on medications or reactive treatments.
Skin barrier protection through gentle cleansing routines, appropriate moisturizing, and avoidance of known irritants creates foundational defense against spongiotic changes. Using lukewarm water, fragrance-free products, and immediate post-bath moisturizing helps maintain healthy skin function.
Environmental trigger identification through systematic observation and testing allows people to avoid substances and situations that trigger their specific patterns of spongiotic dermatitis. Common triggers include certain fabrics, cleaning products, weather conditions, and stress situations.
Immune system support through adequate sleep, regular exercise, stress management, and nutritional optimization helps maintain the body’s natural ability to regulate inflammatory responses and repair skin damage. These lifestyle factors significantly affect condition severity and treatment response.
Regular dermatological monitoring allows for early intervention when symptoms begin developing, preventing progression to severe stages that require more aggressive treatments and carry higher complication risks. Professional guidance helps optimize prevention strategies and treatment approaches.
Living successfully with spongiotic dermatitis requires comprehensive understanding
Managing spongiotic dermatitis effectively involves developing deep understanding of personal trigger patterns, symptom characteristics, and treatment responses while building sustainable lifestyle practices that support long-term skin health and overall wellbeing. This comprehensive approach addresses both immediate symptom relief and long-term condition management.
Educational investment in understanding the condition’s mechanisms, treatment options, and prevention strategies empowers individuals to make informed decisions about their care while working effectively with healthcare providers to optimize outcomes. Knowledge becomes a powerful tool for condition management.
Support system development including healthcare professionals, family members, and potentially support groups provides essential resources for managing challenging flares and maintaining motivation for long-term care routines. Chronic skin conditions affect entire social networks.
Lifestyle adaptation that incorporates skin-friendly practices into daily routines creates sustainable approaches to condition management that don’t feel burdensome or restrictive. Small consistent changes often prove more effective than dramatic lifestyle overhauls.
The journey with spongiotic dermatitis involves learning to balance active management with acceptance of the condition’s chronic nature, finding ways to maintain quality of life while protecting skin health and preventing complications that could affect long-term wellbeing and happiness.