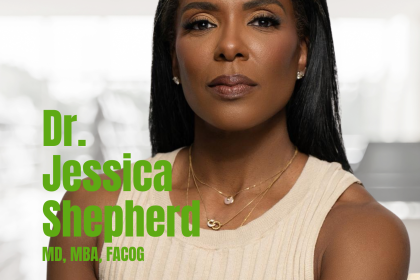
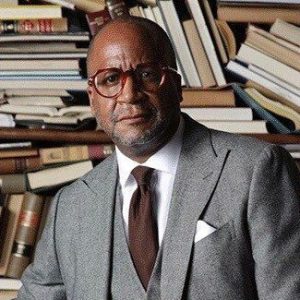
Dr. Derek J. Robinson serves as vice president and chief medical officer at Blue Cross and Blue Shield of Illinois, where he is responsible for clinical leadership, care management operations, and the Institute for Physician Diversity. Previously, Dr. Robinson was vice president at Health Care Service Corporation (HCSC) where he established the Enterprise Quality and Accreditation department and was responsible for clinical quality performance, health plan accreditation, and related operations across multiple states. He established the HCSC Health Equity Steering Committee and served as chairman from 2015 to 2021.
Why did you choose your profession?
When I started as a medical student, I thought I was going to go into family practice. I wanted to be a pillar to the community, I wanted to take care of people from cradle to grave. And as part of that medical school education process, you get a chance to go through several different rotations and experience different types of specialties within medicine. One of the things that I’ve learned in the emergency department was it was sort of ground zero for health care within the medical system, at least in the sense that you get a chance to take care of patients from all walks of life, all socio-demographic backgrounds, ranging from minor things that come up to major things. That variety, and the pace of that work, I found to be stimulating, and a calling to me. Certainly, over the years, I’ve seen a lot of things as an emergency medicine physician that have stimulated my work, not only in the ER, but actually beyond the ER. You see many things that are working in the healthcare system, and many of the things that are broken; not only just in a healthcare system but in society, that impacts the need for individuals to need health care. Figuring out how to address those things on a local and national level has been a product of that experience.
In terms of knowing what you need to do when you’re in the emergency department, I think one of the most challenging things is realizing that things that may seem urgent, you put them in a big spectrum of all the other things that are going on in the ER, and it may fall down the priority list a bit because you have patients in there that many times may have life-threatening conditions. You typically try to make sure patients are not spending a long time waiting, but you prioritize the delivery of care based on how sick and how ill someone is, and unfortunately, people don’t schedule their emergencies. They don’t come at a very regular pace across the day. You can have times when things are quiet and times when things are really busy, and everybody decided to get deathly ill and come in at the same time. It creates a dynamic experience both for patients as well as for those health care providers that are caring.
What did you learn about yourself during the pandemic?
I went to medical school at Howard University. I was there from 1998 through 2002. Following 911, we had anthrax circulating in the Washington, DC postal system. Anthrax was something we learned about in medical school, but not something that we ever dealt with in terms of treating patients. I remember opening my mail outside of my house with my N95 on because you didn’t know. Those were part of the precautions that people were taking back during that period. At that time, it did strike me that at least working in the emergency room you can be on the front lines of a bioterrorism incident. Another data point during my residency training, I worked as a flight physician and sometimes we transport patients across the globe. I recall being in Singapore in 2004 or 2005 and I took a patient from Chicago to there. When we went into the hospital I think it was tan tuck or tank and we went through a tent outside in a parking lot. They had a SARS epidemic in Asia during that period. And when we got to the hospital and I dropped my patient off at the ICU, one of the things I noticed in the hospital was everybody except me had a mask on. I was like, “Well, what do they know that I don’t know?” This transport came up sort of at the last minute, and I didn’t check out what was going on in that part of the world at the time.
Now, having said those two things I didn’t think that I would experience in my lifetime being a physician and dealing with the type of pandemic that we’ve dealt with since late 2019 and going into 2020. And that certainly I think has caused all healthcare providers to think a lot about their morbidity and mortality, and both what they love to do, but also the risk that comes along with providing that care. I know that in my household, my wife is a physician, and we both had that conversation if something happens to both of us, what do you do with your kids? It was a sobering experience from that perspective, not to mention the uncertainty in terms of the ability to provide effective care to patients early in a pandemic, as we were trying to figure out what was going on, how to keep ourselves safe, and how to prevent other folks from getting ill. I think the energy-sapping process of trying to rebuild trust and communities that had a long-standing distrust of the health care system in the midst of all of the misinformation and disinformation that was circulating about both the virus as well as efforts to get folks vaccinated and to keep them safe. So, in terms of things that I learned from that process, about our healthcare delivery system, is that we certainly need to do a better job of addressing the chronic health disparities that are endemic in the Black and Brown community.
What do you say to that person that hasn’t gotten their yearly checkup at the doctor?
The time to act is now. It’s Minority Health Month, and we’ve got a lot of good reasons to be aware of our health status and to engage in practices that are going to make us healthy. There are a couple of things for us to think about that influence our overall health. Getting your preventive screenings, mammography, colorectal cancer screening, new lung cancer screening, or new guidelines for that if you are a family member or a longtime smoker, prostate cancer screening, screening for high blood pressure: all these things are vitally important to ensure that you have longevity, that you can be productive and work, and that you can maintain the financial security of your family. Let’s just think about what happened in the pandemic, where we were just losing people, losing parents losing grandparents, I mean, not only the impact that it had on the family unit but the financial security of families and generations. Your health is your wealth, so we’ve got to do what we’re supposed to do to remain healthy from that perspective. Those prevention pieces are important. I know folks don’t want to take medicine for high blood pressure, a very common conversation I have when I have the privilege of seeing patients in a year. Hypertension is a silent killer because when you have high blood pressure, you feel the same as you do when you don’t have high blood pressure, and that’s part of the problem: people getting treated.
There are things you can do to address blood pressure without medication, good exercise, weight loss, and modifying your diet. Some people need to be on medications for their blood pressure. It is one of the leading drivers of chronic kidney disease, along with diabetes. When I was in one of the neighborhoods we lived in on the south side of Chicago, there was some new construction on a corner. We got excited. It’s about a decade ago. We thought a new restaurant was coming to the community. And what we later noticed was that it was a dialysis center. And it reminded me of what I was seeing as a healthcare provider, lots of young patients come in and had high blood pressure and ended up on dialysis in their 30s. When you blow your kidneys out, and they’re not working anymore, you’re married to having to get dialysis three days a week, which fundamentally changes your life and your healthcare experience. That is avoidable. So, being attentive to these things around maintaining our health is important. And it starts early. We all can make a difference because we can have these influential conversations with people that we care about, that we spend time with, and it’s important to do that.
We have something called cancer alley in Louisiana. Think about fenceline communities, communities that are adjacent to refineries, and what the implications are for not only lung health but different types of cancers that folks are still trying to figure out. Why are those in high neighborhoods, where you don’t have access to a grocery store with fresh food? So, the only thing you have is the corner store with snacks or the fast food restaurant with lots of fried food that’s high in fat and high in salt. Everything is going to make you obese, have high blood pressure, high cholesterol, all the bad stuff, the disparities that we see come from a lot of that. Another thing you could just think about is these social determinants don’t just pop out, they are connected to those political determinants of health that I talked about earlier. Doing what we’re supposed to do in the healthcare system, getting our screenings, taking care of ourselves, having a voice in your community regarding what’s going on, and how resources are distributed and laws are created is important, and being an advocate for these other variables like educational quality and housing, all those things matter as well, so there’s not just kind of one thing that’s impacting the challenges we see in our community. There’s a whole confluence of items that we’ve got to be actively engaged in and I think that’s the promise of having an engaged, younger generation that’s interconnected, that communicates well, and that has access to information. We’ve got to harness all of these things to ensure that we’re able to improve our community.
Why is it important to share the health histories of our families?
It’s not uncommon for folks to find out somebody died, and they had a different type of cancer, this condition or the other, and you’ll be like, “Well, I didn’t know. I was just talking with him last week, and he didn’t say a word.” We have to talk about what’s going on with our health in a way that’s respectful and protects our privacy but ensures that folks in our family know what risk factors they may have, especially when you think about prostate cancer. So, it’s important for a son or a brother to know if his dad or brother had prostate cancer and at what age they had it because that’ll impact screening for them. Similarly, colorectal cancer, having that in a primary relative, and the age at which they have it are important pieces of information. For women, knowing whether your mother had breast cancer or variant cancer, or knowing a sibling with it is important information to know early on because it impacts your screening approach. You want to be able to bring that information to your doctor. Having some familial or genetic risk factors doesn’t necessarily mean that it’s your destiny, or that it’s going to happen for you. We have both genetic predispositions, but we also have what’s happening in the environment where you are, the behaviors that you make, what’s in the environment, where you live, work, and play, and those things can impact whether the disease may manifest itself.
If we don’t talk about it, we don’t collectively improve our health literacy and our health awareness. Just as we share information about how to be financially healthy, we got to ensure that we are being physically healthy. The other thing that’s important is talking about mental health because it’s a lot of stigma around that. So, we’re not going to feel good every day, you’re going to have some challenges and we need to normalize that that’s the case and also ensure that we are encouraging individuals who may be having extensive challenges with depression or anxiety because we know that the prevalence of that is very high, especially in our young people today. It’s okay to say I’ve got a challenge and it’s okay to ask for help. We should be supportive of each other and not stigmatizing.
How can we approach our mental health?
I would say it’s important having a good relationship with a healthcare provider, physician, or nurse practitioner, so that you can talk about symptoms or concerns that you have. Secondly, if you find that you are having symptoms like excessive sleepiness, decreased appetite, decreased interest in things that you otherwise were interested in, feelings of loneliness, worthlessness, and these are things that are feelings that persist for a long period of time or more than several weeks, those are some signs that you need to talk to somebody about what’s going on. Sometimes folks have changes in their feelings that occur with the seasons. Days get shorter, they go through a little something during that time period, and things resolve and get better later in the year. Sometimes you can see some seasonal affective disorder. The prevalence of anxiety is very high in our young people, so we want to be sensitive to that as well. I think the most important thing is to ask people if they’re okay, and if they’re not, that doesn’t mean that they’re defective or something’s wrong with them. But let’s ensure that we get folks access to the support that they need. One of the silver linings that we’ve seen come out of the pandemic is the ability to have access to therapy and behavioral health services, through telehealth. You don’t have to necessarily go sit on a proverbial couch, you can open your phone or your computer, and access a health resource and do so in the privacy of your own home or wherever you are.
Why is staying active important?
Exercise is important, both from a heart perspective, from a cardiovascular perspective, as well as from a muscle strength perspective, and keeping your bones nice and strong as well. Those three descriptions cover all age categories. But you want to be active at least 30 minutes a day, on average, across a week. You might decide that you’re going to do an hour every other day of vigorous exercise, which includes getting your heart rate up as well as some resistance exercise that helps you build your strength, as you get into middle age. When you start getting into your 30s and 40s it’s important to ensure that your core strength is good. One of the most common complaints that individuals have in the healthcare system is back pain. When you think about the years when you’re probably most active, it is when you’re young, when you’re playing sports and other activities. And then you get into your 20s, and then your 30s, and you’re less active. You lose some of that core strength. So, you’re more likely to develop some injuries from lifting things or falling. Being attentive to maintaining and building your core strength is going to be important to help prevent injuries. Exercise is tremendously important. It can help with reducing high blood pressure, it can help with keeping your weight appropriate. These are things that also can help reduce your risk of developing diabetes. For women in their middle age, and as they progressed to get older, resistance training and exercise can also help with bone strength and reduce the risk of developing osteoporosis.