Joint health becomes increasingly important as we age, with approximately 24% of all adults in the United States experiencing joint discomfort that affects daily activities. While some degree of joint change is inevitable with aging, research shows that proactive measures can significantly influence how our joints function in later years. This comprehensive guide explores evidence-based strategies to protect your joints throughout the aging process.
Why joint health matters more with age
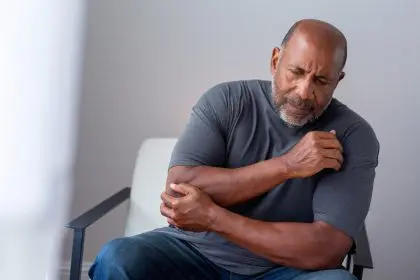
Our joints—the connections between bones that provide support and help us move—undergo natural changes as we age. The cartilage that cushions joints gradually thins, synovial fluid (which lubricates joints) may decrease, and supporting ligaments and tendons become less elastic. These changes can lead to stiffness, discomfort, and reduced mobility that affects quality of life.
Joint issues impact more than just physical comfort; they can significantly affect independence and mental health. Research indicates that adults with chronic joint problems experience higher rates of depression and anxiety, particularly when mobility becomes limited. Preserving joint function thus protects both physical capabilities and psychological wellbeing.
Genetic factors influence joint health, but lifestyle choices play an equally important role. Studies of identical twins demonstrate that environmental factors and personal habits can significantly impact how joints age, even among those with identical genetic makeup. This evidence underscores that joint degeneration isn’t entirely predetermined—our daily choices matter.
1. Maintain a joint-friendly weight
Among all strategies for joint protection, weight management may have the most substantial impact, particularly for weight-bearing joints like knees, hips, and spine. Research demonstrates that each pound of excess weight places approximately four pounds of extra pressure on the knees during walking activities.
The relationship between weight and joint stress follows a multiplier effect. A person who is 10 pounds overweight experiences an additional 40 pounds of pressure on their knees with each step. This mechanical stress accelerates wear and tear on joint cartilage over time.
Beyond mechanical stress, metabolic factors also connect weight and joint health. Fat tissue produces inflammatory compounds called cytokines that can increase overall body inflammation, potentially contributing to joint deterioration. Maintaining a healthy weight helps minimize both the physical pressure and the inflammatory environment that can damage joints.
For those currently carrying excess weight, even modest weight loss shows benefits. Studies indicate that losing just 10% of body weight can reduce joint pain by up to 50% in those with existing joint issues. Small, sustainable changes typically yield better long-term results than drastic weight loss attempts.
2. Prioritize low-impact exercise
Regular physical activity supports joint health through multiple mechanisms. Exercise strengthens the muscles surrounding joints, improves flexibility, enhances circulation to joint tissues, and helps maintain healthy body weight. However, choosing the right types of exercise becomes increasingly important with age.
Low-impact activities provide cardiovascular and strength benefits without excessive joint stress. Swimming and water exercise stand out as particularly joint-friendly options, as water provides resistance while simultaneously supporting body weight. Research shows that aquatic exercise can improve function and reduce discomfort in those with joint issues while building strength and cardiovascular health.
Walking, properly fitted stationary cycling, elliptical training, and tai chi also offer excellent low-impact options. These activities strengthen supporting muscles around joints while minimizing impact forces.
Consistency matters more than intensity. Studies show that moderate exercise performed regularly provides greater joint protection than occasional intense workouts, which can actually increase injury risk. Aim for 150 minutes of moderate activity weekly, divided into manageable sessions.
3. Build muscle to support joints
Muscle strength plays a crucial role in joint protection. Strong muscles help absorb shock that would otherwise be transmitted to joints and provide stability that prevents excessive joint movement and potential damage.
Targeted strengthening exercises for muscles surrounding vulnerable joints can significantly reduce joint stress. For instance, strengthening quadriceps can reduce knee pain by as much as 30% in some cases, according to clinical research. Similarly, core strengthening helps protect the spine from excessive stress.
Resistance training doesn’t necessarily require heavy weights or specialized equipment. Body weight exercises, resistance bands, and light dumbbells can effectively build supporting muscles with minimal joint stress. Proper form always takes precedence over the amount of resistance used.
Including functional exercises that mimic everyday movements—such as squats, modified lunges, and step-ups—helps build practical strength that translates to daily activities. Begin with 2-3 strength sessions weekly, allowing 48 hours between workouts for the same muscle groups to recover.
4. Maintain mobility and flexibility
Joint mobility depends not just on the joint itself but on the flexibility of surrounding soft tissues. Regular stretching helps maintain proper length-tension relationships in muscles, reducing pull on joint structures and allowing fuller range of motion.
Static stretching, where a position is held for 30-60 seconds, most effectively improves flexibility when performed after muscles are warm. Dynamic stretching, involving gentle movement through a range of motion, works well as part of a warm-up routine.
Yoga combines flexibility with strength in ways particularly beneficial for joint health. Research indicates that regular yoga practice improves function and reduces discomfort in those with joint concerns. The mindfulness component of yoga also helps practitioners notice and respect their body’s limits, reducing injury risk.
Daily movement matters as much as formal stretching sessions. Frequently changing positions and avoiding prolonged static postures prevents stiffness and promotes circulation to joint tissues. Aim to change positions at least every 30 minutes during sedentary activities.
5. Focus on nutrient-rich anti-inflammatory foods
Dietary choices influence joint health through their impact on inflammation, body weight, and provision of nutrients needed for tissue repair. Research increasingly points to specific dietary patterns that may support joint function.
Mediterranean-style eating patterns show particular promise for joint health. These diets emphasize olive oil, fatty fish, nuts, fruits, vegetables, and whole grains while limiting processed foods and added sugars. Studies associate Mediterranean eating patterns with reduced inflammatory markers and lower rates of joint problems.
Specific nutrients and food components warrant special attention:
Omega-3 fatty acids found in fatty fish, walnuts, and flaxseeds demonstrate anti-inflammatory properties that may help protect joints. Regular consumption of these foods correlates with lower levels of inflammatory markers in the bloodstream.
Antioxidant-rich fruits and vegetables, particularly those with deep colors like berries, dark leafy greens, and orange vegetables, combat oxidative stress that contributes to joint tissue damage.
Vitamin D and calcium work together to maintain bone strength, which directly impacts joint function. While dairy products provide both nutrients, fatty fish, fortified foods, and brief sun exposure also contribute to vitamin D levels.
Collagen, a protein abundant in bone broth, chicken skin, and fish, provides building blocks for cartilage repair. Some research suggests consuming collagen may support joint tissue maintenance, though more studies are needed.
Equally important is limiting pro-inflammatory foods including highly processed items, excessive added sugars, and refined carbohydrates, which may increase inflammatory markers throughout the body.
6. Protect joints during daily activities
How we perform everyday movements significantly impacts cumulative joint stress. Using proper body mechanics reduces joint strain during daily activities and helps prevent repetitive stress injuries.
When lifting objects, maintain proper spine alignment by bending at the knees and hips rather than the waist. Keep items close to your body to reduce leverage forces on the spine. Whenever possible, push rather than pull heavy objects to minimize strain.
Ergonomic adjustments to home and work environments pay long-term dividends for joint health. Properly positioned computer monitors, supportive chairs, and appropriate work surface heights reduce habitual strain on necks, shoulders, and wrists. Using larger joints for tasks when possible—such as carrying bags on shoulders rather than with fingers—distributes force over greater surface area.
Proper footwear provides a foundation for joint alignment throughout the body. Shoes with adequate arch support and cushioning appropriate for specific activities help absorb impact that would otherwise transmit to ankles, knees, and hips. Research shows that supportive, properly fitted footwear reduces joint stress during walking by up to 15% compared to worn or inappropriate shoes.
Rest and activity cycling proves essential for joint protection. Even during periods of sustained activity, brief breaks to change positions and allow momentary recovery help reduce cumulative stress. The “10-minute rule”—taking a short movement break every hour during sedentary activities—promotes joint fluid circulation and prevents stiffness.
7. Consider joint-supporting supplements
While nutrition from whole foods provides the foundation for joint health, certain supplements show promise for additional support. These should complement rather than replace foundational lifestyle approaches.
Glucosamine and chondroitin sulfate, compounds naturally found in joint cartilage, rank among the most studied joint supplements. Research results have been mixed, but some studies suggest these supplements may slow cartilage deterioration and reduce discomfort, particularly when used consistently over time.
Omega-3 fatty acid supplements provide an alternative source of these anti-inflammatory compounds for those who don’t regularly consume fatty fish. Look for products with verification of purity and potency from independent testing organizations.
Turmeric contains curcumin, a compound with notable anti-inflammatory properties. While the body doesn’t easily absorb curcumin, formulations that include black pepper extract (piperine) enhance absorption up to 2,000%. Some studies show turmeric extracts may reduce joint discomfort comparable to over-the-counter pain relievers in some individuals.
Vitamin D supplementation warrants consideration for those with limited sun exposure or dietary intake, as deficiency correlates with increased joint problems. Blood testing provides the most accurate assessment of vitamin D status to guide appropriate supplementation.
Before starting any supplement regimen, consult healthcare providers, particularly if taking medications or managing health conditions. Quality matters significantly with supplements, as this industry has less regulatory oversight than pharmaceuticals.
When to seek professional guidance
While preventive strategies benefit everyone, certain situations warrant professional evaluation for joint concerns. Seeking timely care often leads to more effective interventions with better outcomes.
Persistent joint discomfort lasting more than two weeks, especially when accompanied by swelling, redness, or warmth, deserves medical attention. These symptoms may indicate inflammatory conditions requiring specific treatment approaches.
Sudden changes in joint function, including reduced range of motion or instability, could suggest structural issues that benefit from proper diagnosis and targeted interventions.
Joint discomfort significantly affecting sleep, daily activities, or quality of life indicates the need for comprehensive evaluation regardless of the duration of symptoms.
Family history of certain joint conditions increases risk, making preventive consultations with healthcare providers valuable for developing personalized protection strategies.
Healthcare professionals specializing in joint health include rheumatologists, orthopedic specialists, physical therapists, and sports medicine practitioners. Primary care providers can offer initial evaluation and appropriate referrals when needed.
Prevention versus intervention
Research consistently demonstrates that preventive approaches to joint health prove more effective than reactive treatments after problems develop. The joint protection strategies outlined here benefit everyone, regardless of current joint status or age.
For those already experiencing joint discomfort, these same strategies often complement medical treatments for better outcomes. Even with existing joint changes, evidence shows that appropriate exercise, weight management, and anti-inflammatory dietary patterns can significantly improve function and reduce symptoms.
The cumulative nature of joint stress means that even small improvements in daily habits yield significant benefits over time. Each step-saving technique, ergonomic adjustment, or nutritious meal choice contributes to the long-term project of joint protection.
Joint aging isn’t entirely preventable, but its progression and impact remain highly modifiable. With consistent application of these evidence-based strategies, many adults maintain comfortable, functional joints well into their later decades, supporting active, independent lifestyles throughout the aging process.