The essential guide to understanding, preventing, and responding to food allergies in children
Food allergies have become increasingly common in American households, affecting between 4-8% of children nationwide. For parents, navigating this medical condition requires vigilance, education, and preparation. The immune system’s reaction to certain foods can range from mild discomfort to life-threatening emergencies, making proper management essential for both physical safety and emotional wellbeing.
With cow’s milk, peanuts, tree nuts, soy, eggs, wheat, fish, and shellfish ranking as the most common triggers, families must adapt daily routines and social interactions around these dietary restrictions. The good news is that with proper strategies, children with food allergies can lead full, active lives while staying safe.
Identifying true food allergies in children
Many parents mistake food intolerances for allergies, but the distinction is crucial. True food allergies involve the immune system and can potentially cause severe reactions. Intolerances, while uncomfortable, typically cause digestive issues without involving immune responses.
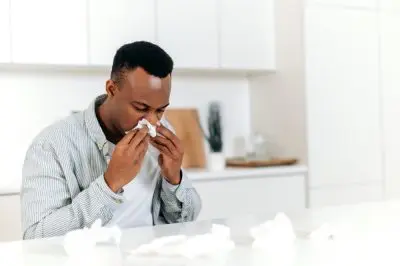
Symptoms of genuine food allergies can develop within minutes or up to two hours after eating and may include skin reactions like hives or eczema flare-ups, digestive problems including vomiting or diarrhea, and respiratory symptoms such as wheezing or nasal congestion. In severe cases, anaphylaxis can occur, presenting as throat tightening, severe drop in blood pressure, and breathing difficulties.
If you suspect your child has a food allergy, documenting reactions thoroughly helps medical professionals make accurate diagnoses. Note what foods were consumed, how quickly symptoms appeared, and their severity. This information proves invaluable during medical consultations and helps distinguish between true allergies and other conditions.
The diagnostic process typically begins with a detailed medical history, followed by specific testing methods. Skin prick tests introduce tiny amounts of potential allergens under the skin to observe reactions. Blood tests measure immune antibodies related to specific foods. In some cases, oral food challenges may be conducted under medical supervision, where small amounts of suspect foods are consumed to monitor reactions.
Early diagnosis allows for proper management plans and emergency preparations, significantly reducing risks associated with accidental exposure. Many children outgrow certain allergies, particularly to milk, eggs, soy, and wheat, making regular reassessment with healthcare providers worthwhile.
Creating an effective allergy action plan
Every child with food allergies needs a comprehensive action plan that outlines specific steps for various scenarios. This written document serves as a roadmap for parents, school staff, babysitters, and other caregivers, ensuring consistent response to potential allergic reactions.
The plan should clearly identify the child’s allergens, detail their typical reaction symptoms, and provide explicit instructions for medication administration. For children at risk of anaphylaxis, the plan must specify when and how to use emergency epinephrine auto-injectors, commonly known as EpiPens.
Make multiple copies of this plan and distribute them to all relevant adults in your child’s life. Update the plan regularly as medications change or if new allergies develop. Some parents find it helpful to include a recent photo of their child on the plan, particularly for school settings where substitute teachers may not recognize the child.
The most effective plans include emergency contact information, healthcare provider details, and specific instructions for post-epinephrine actions, such as calling emergency services and notifying parents. Many allergists provide standardized forms that cover all critical information, though you may need to customize these for your child’s specific situation.
Remember that action plans work best when all caregivers receive proper training in implementing them. Consider scheduling demonstrations of auto-injector use and walking through various scenarios with babysitters, teachers, and family members to ensure everyone feels confident in responding to an emergency.
Essential medical tools and medications
For children with severe food allergies, certain medical tools can literally become lifesavers. Epinephrine auto-injectors top this list, delivering a measured dose of epinephrine to counteract anaphylactic reactions. These devices come in different dosages based on a child’s weight, with specific training required for proper administration.
Always keep at least two auto-injectors available, as a second dose may be necessary if symptoms don’t improve or they return before emergency medical help arrives. Check expiration dates regularly and replace as needed. Remember that temperature extremes can affect medication potency, so avoid leaving auto-injectors in hot cars or freezing environments.
Antihistamines play a supporting role in allergy management, potentially helping with mild symptoms like hives or itching. However, they should never replace epinephrine for severe reactions. Your child’s healthcare provider can recommend appropriate antihistamine types and dosages for your situation.
Some families find medical alert jewelry valuable for communicating about allergies when children are away from parents. These bracelets or necklaces quickly inform others about specific allergies and the potential need for emergency intervention.
Emerging technologies now include smartphone apps that track reactions and medication usage, while some auto-injectors connect to phones to alert emergency contacts when used. While helpful, these technological aids should supplement rather than replace traditional action plans and communication strategies.
Mastering food label literacy
Preventing allergic reactions begins with knowing exactly what ingredients enter your child’s body. Food manufacturers in the United States must clearly identify major allergens on packaged food labels, but understanding these labels requires practice and attention to detail.
The Food Allergen Labeling and Consumer Protection Act requires clear identification of the eight major food allergens: milk, eggs, fish, shellfish, tree nuts, peanuts, wheat, and soy. However, manufacturers may use different terminology that requires familiarity. For instance, casein and whey indicate milk ingredients, while albumin suggests egg content.
Beyond the ingredients list, watch for “Contains” statements that summarize major allergens present in the product. Also important are “May contain” or “Processed in a facility with” warnings that indicate potential cross-contamination risks. For highly sensitive individuals, even trace amounts from shared equipment can trigger reactions.
When facing unfamiliar products or unclear labels, contact manufacturers directly with specific questions about ingredients and manufacturing processes. Most companies provide consumer hotlines specifically for allergy inquiries. Some families find shopping apps helpful for scanning barcodes to quickly identify potential allergens in products.
Remember that ingredients in familiar products can change without notice, making it essential to check labels every time – even for products previously deemed safe. This vigilance becomes particularly important during holiday seasons when limited-edition variants of regular products may contain different ingredients.
Navigating school and social settings
Children spend significant time in environments beyond parental control, making clear communication with schools, activity leaders, and other parents essential for safety. Begin conversations about accommodations well before the school year starts, preferably with face-to-face meetings that establish relationships with key staff members.
Federal laws, including the Americans with Disabilities Act, provide certain protections for children with severe food allergies in school settings. Many schools develop individualized healthcare plans that outline specific accommodations, potentially including allergen-free tables, classroom food restrictions, or staff training requirements.
For younger children, consider providing safe snacks that can be stored at school for unexpected celebrations or activities involving food. Creating a small, decorated “safe treat box” can help children feel included rather than isolated during these events.
Social gatherings present particular challenges for families managing food allergies. When possible, offer to bring safe dishes to share at parties, allowing your child to participate without risk. For sleepovers or playdates, having direct conversations with host parents about allergens, cross-contamination risks, and emergency procedures helps prevent dangerous situations.
Birthday parties often center around food that may contain allergens. Some families find it helpful to bring comparable safe alternatives, such as cupcakes that resemble the birthday cake. Communicating with host families ahead of time allows for planning that includes rather than excludes children with dietary restrictions.
Remember that balance matters – while safety remains the priority, working toward inclusion rather than isolation serves your child’s emotional wellbeing. Creative solutions often allow participation while maintaining necessary precautions.
Teaching children age-appropriate responsibility
As children grow, gradually shifting appropriate levels of responsibility to them builds confidence and safety skills. Even preschoolers can learn simple concepts like asking adults about food ingredients before eating and understanding which foods are “safe” versus “unsafe” for them personally.
Elementary-aged children can begin learning to read basic food labels with supervision and understand the importance of not sharing food with classmates. By middle school, many children become capable of carrying their own auto-injectors and communicating their needs directly to adults in various settings.
Practice role-playing scenarios help children develop confidence in declining unsafe foods or explaining their allergies to others. Phrases like “No thank you, I have food allergies” or “I need to check with my mom first” should become automatic responses when offered unfamiliar foods.
Creating age-appropriate visuals helps younger children identify their allergens. Picture cards showing foods to avoid, refrigerator charts with safe/unsafe categories, or special placemats with allergen information provide constant visual reminders that reinforce safety habits.
While fostering independence, maintain appropriate oversight based on your child’s maturity level and the severity of their allergies. Some children develop responsibility more quickly than others, and high-risk allergies may require closer supervision even as children mature.
The goal remains preparing children to eventually manage their allergies independently as adults. Each small step toward self-management builds both practical skills and the confidence needed to navigate the world safely with food allergies.
Addressing psychological impacts of food allergies
The emotional aspects of living with food allergies often receive less attention than physical management, yet they significantly affect quality of life. Children with food allergies may experience anxiety about potential reactions, feelings of isolation during food-centered activities, or frustration with necessary restrictions.
Parents can help by acknowledging these feelings rather than dismissing them. Create space for conversations about the challenges while also highlighting coping strategies. Emphasize what your child can do rather than focusing exclusively on limitations.
Certain developmental stages present unique challenges. Teenagers often face increased pressure around social eating and may take risks to avoid feeling different from peers. Open communication about these pressures, without judgment, helps teens develop strategies for managing social situations while maintaining safety.
Consider connecting with support groups where children can meet others with similar experiences. Organizations like Food Allergy Research & Education (FARE) offer resources for finding local support networks where families share strategies and emotional support.
For children experiencing significant anxiety or social difficulties related to food allergies, professional mental health support may prove beneficial. Cognitive-behavioral techniques can help address specific fears, while family therapy sometimes helps resolve tensions that develop around food restrictions within the home.
Remember that your attitude as a parent significantly influences how your child perceives their allergies. Approaching management with confidence rather than constant fear helps children develop resilience and a positive outlook despite their dietary restrictions.
Staying informed about emerging treatments
The landscape of food allergy treatment continues evolving, with promising new approaches emerging in recent years. While strict avoidance remains the primary management strategy, several interventions show potential for reducing severity or inducing tolerance to specific allergens.
Oral immunotherapy (OIT) involves consuming gradually increasing amounts of allergens under medical supervision to build tolerance. While not a cure, successful OIT can protect against reactions from accidental exposures by raising the threshold amount needed to trigger symptoms.
Epicutaneous immunotherapy applies small amounts of allergens to the skin through special patches, potentially desensitizing the immune system with fewer side effects than oral approaches. Research continues on this less invasive method, particularly for younger children.
Biologics represent another frontier, with medications designed to modify immune responses at the cellular level. Some target specific antibodies involved in allergic reactions, potentially reducing reaction severity across multiple allergens simultaneously.
Microbiome research explores connections between gut bacteria and food allergies, with some studies suggesting probiotic supplements may help prevent or treat certain allergies by promoting healthy immune development.
While exciting, these approaches remain primarily in research phases or available only through specialized allergy centers. Families interested in emerging treatments should discuss options with their allergists, who can provide guidance on clinical trials or treatment availability based on individual circumstances.
Stay connected with reputable organizations that provide updates on research developments, such as academic medical centers with specialized food allergy programs. These resources help families make informed decisions as new options become available, always balancing potential benefits against risks.
Food allergies present real challenges for children and their families, but with proper management strategies, affected children can thrive. By creating comprehensive plans, teaching age-appropriate skills, addressing emotional impacts, and staying informed about treatment advances, parents provide their children with both safety and the confidence to navigate the world despite dietary restrictions. The vigilance required may feel overwhelming initially, but most families develop routines that eventually become second nature, allowing focus to shift from limitations to possibilities.