When spring flowers bloom or fall leaves scatter, millions reach for tissues to combat the familiar sneezing and itchy eyes of seasonal allergies. Yet a lesser-known consequence lurks beneath these obvious symptoms: body aches and muscle pain that many sufferers mistakenly attribute to other causes.
This connection between allergies and physical discomfort remains underrecognized, even among those who experience it regularly. While most associate allergies with respiratory and sinus symptoms, the body’s response to allergens can trigger widespread effects that manifest as soreness, stiffness, and general malaise.
Understanding this relationship helps explain why some individuals feel physically exhausted during allergy flares. The immune system’s reaction to harmless substances—whether pollen, pet dander, or certain foods—sets off a cascade of responses that extend far beyond the respiratory system, affecting muscles, joints, and overall energy levels.
For those experiencing unexplained aches during peak allergy seasons, this connection offers valuable insight into managing their symptoms effectively. Addressing the root cause—the allergic reaction—often provides relief from both the obvious symptoms and the accompanying discomfort.
6 ways allergies trigger body aches and muscle pain
While many consider allergies primarily a respiratory issue, several mechanisms connect these immune responses to physical pain and discomfort throughout the body:
1. Widespread inflammation affects muscles and joints
The fundamental process behind allergic reactions—inflammation—extends beyond local symptoms. When the immune system identifies an allergen as threatening, it releases chemicals like histamine and cytokines to combat the perceived invader. This inflammatory response, while intended to protect the body, creates collateral damage.
These inflammatory chemicals circulate throughout the bloodstream, affecting tissues far from the initial reaction site. For individuals with existing inflammatory conditions like arthritis or fibromyalgia, this additional inflammation can significantly amplify pain levels.
The resulting muscle soreness resembles post-exercise discomfort or the early stages of illness, creating a persistent, hard-to-pinpoint achiness. This systemic inflammation explains why allergy sufferers often experience discomfort in areas seemingly unconnected to their respiratory symptoms.
2. Repetitive coughing and sneezing strains the body
The physical act of frequent coughing and sneezing places tremendous strain on core muscles. A single sneeze involves abdominal muscles, intercostal muscles between the ribs, and the diaphragm contracting forcefully. When these actions repeat dozens or even hundreds of times daily during allergy season, the resulting muscle fatigue creates genuine pain.
This repetitive strain particularly affects the chest, back, and abdominal muscles. The unexpected, forceful nature of sneezing allows no time for proper muscular preparation, increasing the likelihood of strain or minor injury with each episode.
Additionally, the hunched posture many adopt when dealing with persistent coughing adds further strain to the back and neck. Over time, this altered positioning contributes to misalignment and muscle tension that compounds the direct effects of the allergic response.
3. Rib inflammation mimics serious chest pain
One particularly concerning manifestation of allergy-related discomfort involves inflammation of the cartilage connecting the ribs to the breastbone—a condition called costochondritis. This painful condition often creates sharp chest pain that worsens with deep breathing, coughing, or physical activity.
The connection to allergies comes from both direct inflammatory effects and the physical strain of persistent coughing. As the cartilage becomes irritated, the resulting pain can radiate throughout the chest wall and sometimes extend to the back and abdomen.
For many experiencing this symptom, the chest pain creates significant anxiety due to its resemblance to cardiac issues. Understanding that allergies can trigger this type of discomfort helps differentiate between concerning medical emergencies and treatable inflammatory responses.
4. Sinus pressure creates radiating pain
Sinus congestion represents one of the most common allergy symptoms, yet its effects extend beyond the face. The pressure created by inflamed, fluid-filled sinuses triggers nerve pathways that connect to other parts of the body, resulting in referred pain that can manifest far from the sinuses themselves.
This pain often radiates from the face to the head, neck, shoulders, and sometimes even down the back. The constant pressure and associated headaches contribute significantly to the overall feeling of physical discomfort during allergy seasons.
Additionally, many allergy sufferers unconsciously tense their facial and neck muscles in response to sinus discomfort, creating a secondary source of muscle strain that compounds the direct effects of the allergic reaction.
5. Sleep disruption intensifies pain perception
Allergies drastically impact sleep quality, creating a vicious cycle that worsens physical discomfort. Congestion makes breathing difficult at night, while post-nasal drip triggers coughing that interrupts sleep cycles. This disrupted sleep prevents the body’s natural overnight healing processes.
Research consistently shows that poor sleep lowers pain thresholds and amplifies pain perception. Even a few nights of interrupted rest can significantly increase sensitivity to discomfort, making existing aches feel more severe.
Many allergy medications compound this issue by either causing drowsiness that results in poor-quality sleep or containing stimulants that make falling asleep difficult. This medication-induced sleep disruption further contributes to physical discomfort and fatigue.
6. Fatigue manifests as physical discomfort
The combination of inflammatory responses, disrupted sleep, and constant physical strain creates profound fatigue in allergy sufferers. This exhaustion often manifests physically as muscle weakness, generalized soreness, and increased sensitivity to discomfort.
The immune system’s constant activation consumes significant energy resources, leaving less available for normal physical recovery and function. This energy deficit affects muscle performance and recovery, creating a persistent feeling of physical depletion.
This fatigue-related discomfort often lingers even when more obvious allergy symptoms subside, creating the impression of a prolonged illness rather than an allergic reaction. Understanding this connection helps explain why recovery from severe allergy flares can take weeks rather than days.
Managing the physical pain of allergies
Effectively addressing allergy-related body aches requires a two-pronged approach—treating the allergic reaction itself while also managing the resulting physical discomfort:
Identifying specific triggers represents the first step toward relief. Modern allergy testing can pinpoint exactly which substances trigger immune responses, allowing for targeted avoidance strategies. For seasonal allergies, tracking pollen counts helps predict high-risk days when symptoms might intensify.
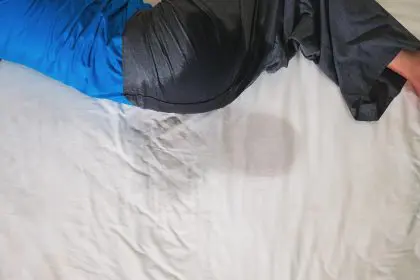
Environmental modifications make a significant difference in symptom severity. High-efficiency air filters, regular cleaning to reduce dust accumulation, and keeping windows closed during peak pollen seasons all reduce allergen exposure. For those allergic to dust mites, specialized mattress and pillow covers provide protection during sleep.
Anti-inflammatory treatments address both the allergy symptoms and the resulting discomfort. While antihistamines help with obvious symptoms like sneezing and itching, they often don’t adequately address the inflammatory component driving body aches. Adding anti-inflammatory approaches—whether medication or natural alternatives like turmeric or omega-3 supplements—provides more comprehensive relief.
Physical therapy techniques prove surprisingly effective for allergy-related muscle tension. Gentle stretching, particularly targeting the upper back, neck, and chest, helps counteract the strain from coughing and sneezing. Heat application relaxes tense muscles, while cold therapy reduces acute inflammation.
Sleep-focused strategies break the cycle of discomfort and sleep disruption. Using humidifiers to ease breathing, elevating the head to reduce post-nasal drip, and creating optimal sleeping conditions help maximize rest quality. For some, temporarily separating from sleeping partners may prove necessary during severe allergy periods to ensure uninterrupted sleep.
When allergy pain requires medical attention
While most allergy-related discomfort responds to self-care measures, certain situations warrant professional medical evaluation:
Chest pain that feels crushing or comes with shortness of breath requires immediate emergency attention to rule out cardiac causes, even if allergies seem the likely culprit. The similarity between costochondritis and heart attack symptoms makes professional assessment crucial.
Pain accompanied by fever, especially when localized to one area, suggests possible infection rather than allergy effects. Sinus infections, bronchitis, and pneumonia can all develop secondary to prolonged allergy symptoms and require specific treatments.
Muscle weakness that affects daily function, particularly when asymmetrical or progressive, needs evaluation to distinguish between allergy-related fatigue and neurological issues that might coincidentally emerge during allergy season.
Unresponsive symptoms that persist despite appropriate self-care measures indicate the need for medical intervention. Prescription-strength treatments or immunotherapy may provide relief when over-the-counter approaches prove insufficient.
Beyond symptom management: long-term solutions
For those experiencing significant body aches with allergies, several approaches offer longer-term relief:
Immunotherapy—either through injections or newer sublingual options—gradually desensitizes the immune system to specific allergens. While requiring months or years for full effect, this approach addresses the root cause rather than just managing symptoms.
Anti-inflammatory dietary approaches help reduce the body’s overall inflammation levels. Mediterranean-style eating patterns, rich in fruits, vegetables, and omega-3 fatty acids, create a foundation less prone to inflammatory overreactions.
Stress management techniques like meditation, deep breathing, and yoga help modulate immune responses. Chronic stress amplifies inflammatory reactions to allergens, while effective stress management helps maintain a more balanced immune response.
Year-round physical conditioning, particularly core strength development, helps the body better withstand the strain of allergic episodes. Strong, flexible muscles experience less damage from coughing and sneezing, reducing the physical toll of allergy seasons.
Changing how we think about allergies
The connection between allergies and body aches highlights the need to view allergic reactions as whole-body events rather than isolated respiratory issues. This broader understanding allows for more comprehensive treatment approaches that address both the obvious symptoms and their less apparent physical consequences.
For the millions experiencing unexplained aches during high allergy seasons, recognizing this connection offers both explanation and hope. By targeting the allergic response while supporting the body’s recovery from physical strain, most find significant relief from both the respiratory symptoms and the accompanying discomfort.
This integrated approach transforms allergy management from a frustrating, never-ending battle to a more effective strategy that improves overall quality of life. By addressing both the obvious and hidden effects of allergic reactions, even longtime sufferers can experience greater comfort and vitality throughout allergy season.