Heel pain affects millions of Americans daily, transforming simple activities like walking to the mailbox or climbing stairs into uncomfortable ordeals. While occasional foot discomfort might seem like a minor inconvenience, certain warning signs indicate when heel pain requires immediate medical evaluation.
The feet bear the entire weight of the body throughout the day, making them susceptible to various injuries and conditions. Most people experience temporary heel discomfort at some point, often dismissing it as a result of wearing uncomfortable shoes or standing too long. However, persistent or severe heel pain can signal underlying conditions that, left untreated, may lead to chronic problems or permanent damage.
Understanding when heel pain crosses the line from minor annoyance to medical concern empowers individuals to seek appropriate care before conditions worsen. Early intervention often prevents complications and reduces recovery time, making recognition of warning signs essential for maintaining optimal foot health.
1. Pain persists beyond two weeks despite rest
Heel pain that continues for more than two weeks despite adequate rest and basic home care measures warrants professional evaluation. Acute heel pain from overuse or minor strain typically improves within a few days to a week with proper rest, ice application, and avoiding aggravating activities.
When discomfort lingers beyond the expected healing timeframe, it often indicates an underlying condition requiring targeted treatment. Plantar fasciitis, one of the most common causes of heel pain, frequently develops gradually and persists without appropriate intervention. The plantar fascia, a thick band of tissue supporting the arch of the foot, can become inflamed and develop small tears that require specific treatment approaches.
Chronic heel pain may also result from heel spurs, small calcium deposits that form on the heel bone. These bony growths develop over time and can cause significant discomfort, particularly during the first steps after periods of rest. Without proper treatment, heel spurs can worsen and create ongoing mobility issues.
2. Morning pain intensity exceeds normal stiffness
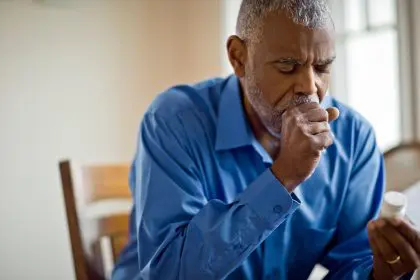
Severe heel pain upon taking the first steps in the morning, particularly pain that causes limping or difficulty bearing weight, requires medical attention. While mild morning stiffness is common as muscles and joints warm up after hours of inactivity, intense heel pain that significantly impacts mobility suggests inflammation or structural problems.
The morning pain associated with plantar fasciitis often feels like stepping on sharp objects or experiencing deep, stabbing sensations in the heel. This occurs because the plantar fascia tightens overnight, and the initial stretching upon standing can aggravate inflamed tissue. When morning pain is so severe that it affects normal walking patterns or requires significant modification of morning routines, professional evaluation becomes necessary.
Achilles tendonitis can also cause severe morning heel pain, particularly in the back of the heel where the Achilles tendon attaches to the heel bone. This condition often develops in active individuals who suddenly increase their exercise intensity or duration without proper conditioning.
3. Swelling accompanies the heel discomfort
Visible swelling around the heel area, particularly when accompanied by warmth or redness, indicates inflammation that requires medical evaluation. Swelling suggests tissue damage or an active inflammatory process that may not resolve with basic home care measures.
Bursitis, inflammation of the small fluid-filled sacs that cushion bones and soft tissues, commonly causes heel swelling. The bursa located between the Achilles tendon and heel bone can become inflamed from repetitive stress, direct trauma, or underlying conditions. When inflamed, this bursa creates noticeable swelling and tenderness at the back of the heel.
Infections, though less common, can also cause heel swelling accompanied by warmth, redness, and sometimes fever. Bacterial infections in the foot require immediate antibiotic treatment to prevent serious complications. Any swelling that develops rapidly or is accompanied by streaking red lines extending up the leg demands emergency medical attention.
4. Pain interferes with daily activities and sleep
Heel pain that disrupts normal daily activities or prevents restful sleep indicates a condition requiring professional treatment. When discomfort forces individuals to modify their walking patterns, avoid certain activities, or wake up during the night due to pain, the condition has progressed beyond what home remedies can effectively address.
Chronic heel pain often creates compensatory movement patterns as individuals unconsciously adjust their gait to minimize discomfort. These adaptations can lead to secondary problems in the knees, hips, or back as other body parts work harder to compensate for altered foot mechanics. Early intervention prevents these cascade effects that can create additional pain and mobility issues.
Night pain, particularly pain that wakes individuals from sleep, often indicates more severe inflammation or nerve involvement. Conditions like tarsal tunnel syndrome, where nerves become compressed as they pass through a narrow space in the ankle, can cause burning or tingling pain that worsens at night when blood flow to the feet decreases.
5. Numbness or tingling sensations develop
The presence of numbness, tingling, or burning sensations in the heel or extending into other parts of the foot suggests nerve involvement that requires immediate medical evaluation. These neurological symptoms can indicate nerve compression, damage, or underlying conditions affecting nerve function.
Tarsal tunnel syndrome occurs when the posterior tibial nerve becomes compressed as it passes through a narrow channel on the inside of the ankle. This compression can cause burning pain, tingling, or numbness that radiates from the heel into the arch and toes. Without proper treatment, nerve compression can lead to permanent damage and chronic pain.
Peripheral neuropathy, often associated with diabetes or other systemic conditions, can also cause heel numbness and tingling. Early detection and management of underlying conditions causing neuropathy can prevent progression and preserve nerve function. Any numbness or tingling in the feet should prompt immediate medical evaluation, particularly in individuals with diabetes or other risk factors for nerve damage.
6. Heel pain follows a traumatic injury
Heel pain that develops after a fall, direct blow to the heel, or sudden twisting motion requires prompt medical evaluation to rule out fractures or other serious injuries. Traumatic heel injuries can cause hairline fractures in the heel bone (calcaneus) that may not be immediately apparent but can lead to long-term complications if not properly treated.
Stress fractures can also develop in the heel bone from repetitive impact, particularly in runners or individuals who suddenly increase their activity level. These small cracks in the bone often cause deep, aching pain that worsens with weight-bearing activities and may not show up on initial X-rays.
Achilles tendon ruptures, though more commonly affecting the back of the ankle, can also cause heel pain and require immediate medical attention. Complete tendon ruptures often cause a sudden, sharp pain followed by inability to point the foot downward or rise up on the toes. Partial ruptures may cause ongoing heel pain with weakness and stiffness.
7. Fever accompanies persistent heel pain
The combination of heel pain with fever, particularly when accompanied by swelling, redness, or warmth, can indicate a serious infection requiring immediate medical attention. Infections in the foot can spread rapidly and cause severe complications if not treated promptly with appropriate antibiotics.
Cellulitis, a bacterial skin infection, can affect the heel area and cause spreading redness, warmth, swelling, and systemic symptoms like fever and chills. This condition requires immediate antibiotic treatment and close monitoring to prevent the infection from spreading to deeper tissues or entering the bloodstream.
Bone infections (osteomyelitis), though less common, can also cause severe heel pain with fever. These deep infections are particularly concerning in individuals with diabetes, compromised immune systems, or circulation problems. Bone infections often require prolonged antibiotic treatment and sometimes surgical intervention to prevent serious complications.
Taking action for heel health
Recognizing these warning signs empowers individuals to seek appropriate medical care before heel pain conditions worsen or cause permanent damage. Early intervention typically results in better outcomes, shorter recovery times, and reduced risk of chronic problems.
Healthcare providers can perform comprehensive evaluations including physical examinations, imaging studies, and specialized tests to determine the exact cause of heel pain. Treatment options range from conservative approaches like physical therapy, orthotics, and medication to more advanced interventions when necessary.
Maintaining foot health through proper footwear, gradual activity progression, and attention to early warning signs helps prevent many heel pain conditions. However, when warning signs appear, prompt medical evaluation ensures optimal outcomes and prevents minor problems from becoming major complications.