Bone cancer represents a serious medical condition that affects thousands of people each year, yet many individuals remain unfamiliar with its characteristics, symptoms, and treatment approaches. Understanding this disease empowers patients and families to recognize warning signs early and make informed decisions about medical care.
Unlike many other cancer types that spread to bones from other organs, primary bone cancer actually originates within bone tissue itself. This distinction proves important for treatment planning and prognosis, as primary bone cancers require different therapeutic approaches than secondary bone cancers that have metastasized from elsewhere.
The complexity of bone cancer stems from the various types of cells within bone tissue that can become malignant. Bones contain multiple cell types including bone-forming cells, cartilage cells, and connective tissue cells, each capable of developing into different cancer varieties with unique characteristics and behaviors.
Early detection significantly improves treatment outcomes for bone cancer patients, making awareness of symptoms and risk factors crucial for optimal results. Modern treatment approaches have dramatically improved survival rates and quality of life for many bone cancer patients when diagnosed promptly.
Types of primary bone cancer
Osteosarcoma represents the most common form of primary bone cancer, typically affecting children, teenagers, and young adults. This aggressive cancer usually develops in the long bones of the arms and legs, particularly around the knee area, and tends to grow rapidly if left untreated.
Ewing sarcoma affects bones and soft tissues, most commonly occurring in children and young adults under age 20. This cancer type often develops in the pelvis, ribs, or long bones and can spread quickly to other parts of the body, making early treatment essential.
Chondrosarcoma develops in cartilage cells and primarily affects adults over age 40. This cancer type grows more slowly than osteosarcoma and Ewing sarcoma, typically occurring in the pelvis, hip, shoulder, or ribs. The slower growth pattern often leads to better treatment outcomes.
Giant cell tumor of bone, while often benign, can sometimes become malignant and cause significant bone destruction. These tumors typically affect adults between ages 20 and 40, most commonly occurring near the ends of long bones close to joints.
Fibrosarcoma and malignant fibrous histiocytoma represent less common bone cancer types that can affect both bones and soft tissues. These cancers typically occur in middle-aged and older adults, often developing in the arms, legs, or jaw bones.
Common symptoms and warning signs
Persistent bone pain represents the most frequent early symptom of bone cancer, often beginning as mild discomfort that gradually worsens over time. This pain typically occurs at night or during rest periods and may not respond well to over-the-counter pain medications.
Swelling and tenderness around the affected bone area often accompany pain symptoms, creating visible lumps or masses that can be felt through the skin. The swelling may develop gradually over weeks or months, becoming more noticeable as the tumor grows.
Fractures occurring with minimal trauma or during routine activities can indicate weakened bones from cancer involvement. These pathological fractures often happen in bones that would normally withstand everyday stresses without breaking.
Fatigue and unexplained weight loss may develop as bone cancer progresses, particularly when the disease spreads to other parts of the body. These systemic symptoms often indicate more advanced disease requiring immediate medical attention.
Limited range of motion in nearby joints can occur when bone cancer affects areas close to major joints like the knee, hip, or shoulder. This restriction typically worsens gradually as the tumor grows and affects surrounding tissues.
Risk factors and potential causes
Age represents a significant risk factor, with certain bone cancer types showing distinct age patterns. Osteosarcoma primarily affects teenagers and young adults during periods of rapid bone growth, while chondrosarcoma typically occurs in older adults.
Previous radiation therapy exposure increases bone cancer risk, particularly when high doses were administered during childhood cancer treatment. The risk appears years or decades after radiation exposure, requiring long-term monitoring of previously treated patients.
Genetic conditions like Li-Fraumeni syndrome, hereditary retinoblastoma, and Paget disease can predispose individuals to bone cancer development. These rare conditions affect DNA repair mechanisms or bone remodeling processes, increasing malignancy risk.
Pre-existing bone conditions including bone infarcts, chronic osteomyelitis, and fibrous dysplasia may occasionally progress to malignant transformation. Regular monitoring of these conditions helps detect any suspicious changes early.
Previous chemotherapy treatment, particularly with alkylating agents, can increase bone cancer risk later in life. This risk factor highlights the importance of long-term follow-up care for cancer survivors.
Diagnostic procedures and testing
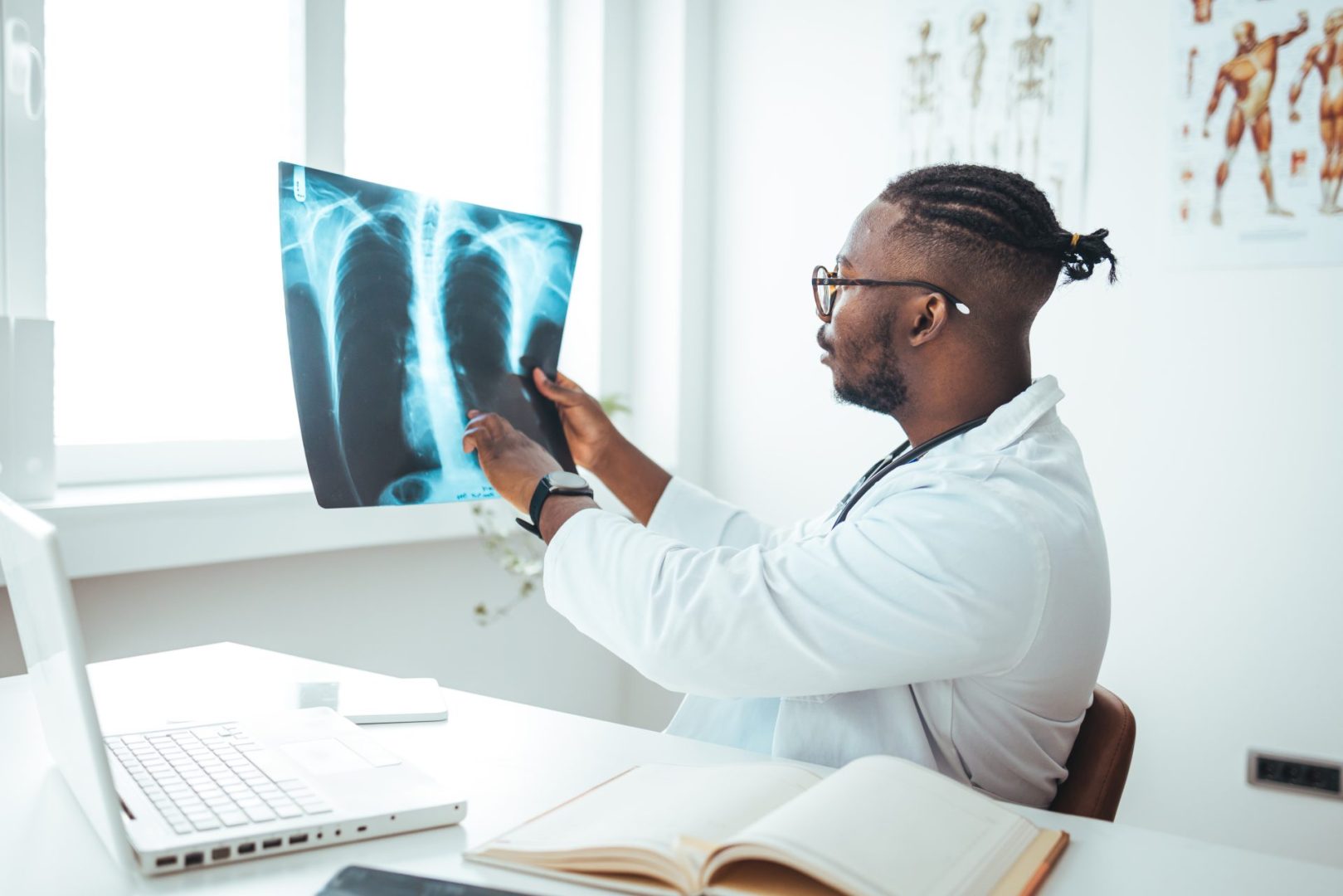
Physical examination begins the diagnostic process, with healthcare providers assessing symptoms, examining affected areas, and evaluating overall health status. This initial evaluation helps determine which additional tests may be necessary.
Imaging studies provide crucial information about tumor location, size, and characteristics. X-rays often reveal bone destruction or abnormal bone formation, while CT scans and MRI provide detailed images of both bone and soft tissue involvement.
Bone scans use radioactive tracers to identify areas of increased bone activity throughout the skeleton, helping determine if cancer has spread to multiple bone sites. This whole-body imaging technique proves particularly valuable for staging purposes.
Biopsy procedures provide definitive cancer diagnosis by examining actual tissue samples under microscopic analysis. Needle biopsies or surgical biopsies may be performed depending on tumor location and accessibility.
Blood tests can reveal elevated levels of certain substances associated with bone cancer, though these findings alone cannot confirm diagnosis. Alkaline phosphatase and lactate dehydrogenase levels may be elevated in some bone cancer cases.
Staging and prognosis factors
Staging systems help determine cancer extent and guide treatment planning by evaluating tumor size, location, and spread to other body areas. The TNM staging system considers tumor characteristics, lymph node involvement, and distant metastases.
Tumor grade reflects how abnormal cancer cells appear under microscopic examination and how quickly they are likely to grow and spread. Higher-grade tumors typically require more aggressive treatment approaches.
Location within the bone affects treatment options and outcomes, with tumors in certain areas proving more challenging to treat surgically. Central locations like the pelvis or spine present greater surgical complexity than peripheral limb locations.
Patient age and overall health status influence treatment tolerance and recovery potential. Younger patients often tolerate intensive treatments better, while older patients may require modified approaches based on other health conditions.
Response to initial treatment provides important prognostic information, with patients showing good response to chemotherapy typically having better long-term outcomes than those with resistant disease.
Treatment approaches and options
Surgical removal represents the primary treatment for most bone cancers, with the goal of completely removing the tumor while preserving as much normal function as possible. Limb-salvage procedures have largely replaced amputation for many patients.
Chemotherapy plays a crucial role in treating aggressive bone cancers like osteosarcoma and Ewing sarcoma, often administered both before and after surgery to shrink tumors and eliminate microscopic disease spread.
Radiation therapy may be used when complete surgical removal proves impossible or to treat cancer that has spread to other areas. Modern radiation techniques allow precise targeting while minimizing damage to surrounding healthy tissues.
Targeted therapy drugs attack specific characteristics of cancer cells, offering new treatment options for certain bone cancer types. These medications work differently than traditional chemotherapy and may have fewer side effects.
Immunotherapy approaches harness the body’s immune system to fight cancer cells, representing an emerging treatment area for bone cancers. These treatments show promise for patients who don’t respond to conventional therapies.
Reconstruction and rehabilitation
Bone reconstruction techniques help restore function and appearance after tumor removal, using metal implants, bone grafts, or artificial joints to replace removed bone sections. Modern reconstruction methods provide excellent functional outcomes for many patients.
Physical therapy plays a vital role in recovery, helping patients regain strength, mobility, and function after surgery and other treatments. Rehabilitation programs are tailored to individual needs and treatment approaches.
Prosthetic devices may be necessary for patients requiring amputation, with modern prosthetics offering remarkable functionality and cosmetic appearance. Training and adjustment periods help patients adapt to prosthetic use.
Occupational therapy helps patients adapt to changes in daily living activities and return to work or school when possible. These services address practical concerns about functioning with treatment-related limitations.
Psychological support addresses the emotional challenges of cancer diagnosis and treatment, helping patients and families cope with fears, uncertainty, and lifestyle changes associated with bone cancer.
Long-term follow-up and monitoring
Regular surveillance imaging monitors for cancer recurrence, with the frequency and type of scans depending on cancer type, stage, and treatment received. Early detection of recurrence allows for prompt intervention.
Functional assessments evaluate how well reconstructed bones and joints are working over time, identifying any problems that might benefit from additional interventions or adjustments.
Late effects monitoring addresses potential long-term complications from treatment, including secondary cancers, heart problems from chemotherapy, or joint issues from radiation therapy.
Quality of life evaluations help healthcare teams understand how treatments have affected patients’ daily lives and identify areas where additional support or interventions might be beneficial.
Lifestyle guidance addresses activities, exercise, and precautions that may be appropriate for bone cancer survivors, helping them maintain optimal health while accommodating any treatment-related limitations.
Prevention and awareness
While most bone cancers cannot be prevented due to unknown causes, awareness of symptoms and risk factors enables earlier detection and treatment. Regular medical care and prompt evaluation of concerning symptoms prove essential.
Genetic counseling may benefit individuals with family histories of bone cancer or known genetic predispositions, helping them understand risks and appropriate monitoring strategies.
Healthy lifestyle choices including regular exercise, adequate nutrition, and avoiding tobacco support overall bone health, though their specific impact on bone cancer prevention remains unclear.
Education about bone cancer symptoms and risk factors helps individuals recognize when medical evaluation is appropriate, potentially leading to earlier diagnosis and better treatment outcomes.
Understanding bone cancer empowers patients and families to actively participate in treatment decisions and advocate for comprehensive care that addresses both medical and quality of life concerns throughout the cancer journey.