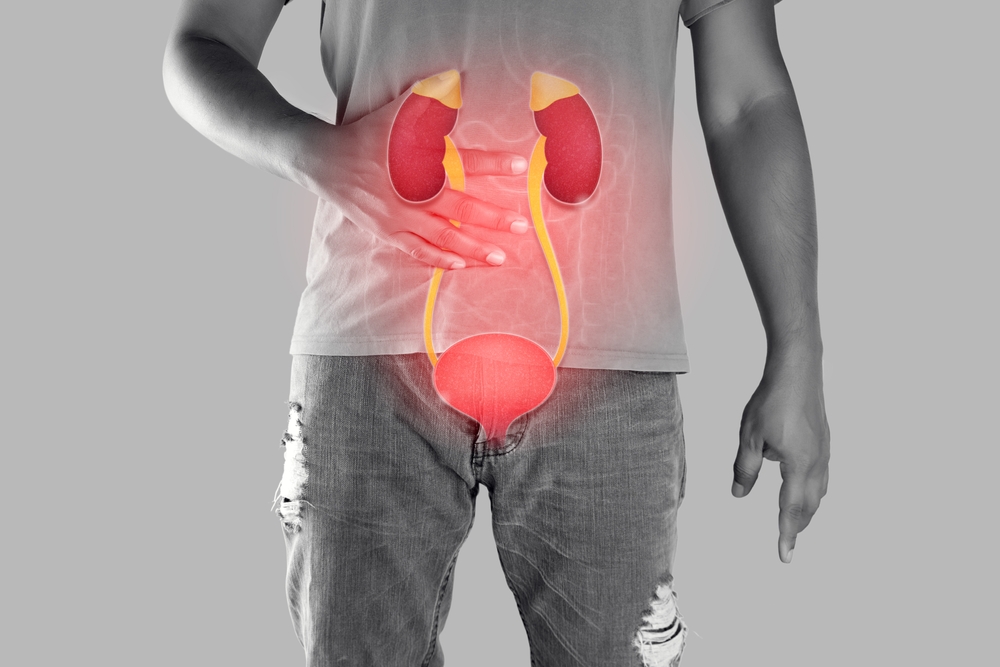
More than 37 million Americans live with chronic kidney disease, yet most remain unaware of their condition until significant damage has already occurred. The silent nature of kidney disease makes it particularly dangerous, as symptoms often don’t appear until kidney function has declined substantially.
What many people don’t realize is that common chronic conditions they may already have are systematically damaging their kidneys every day. Diabetes, high blood pressure, and heart disease create a cascade of physiological changes that slowly but steadily compromise kidney function over months and years.
Understanding these connections empowers individuals to take proactive steps in protecting their kidney health before irreversible damage occurs. The relationship between chronic illnesses and kidney disease represents one of the most critical health challenges of our time, affecting millions of families across the country.
Diabetes transforms kidneys into damaged filters
Type 2 diabetes creates devastating effects on kidney health through a process called diabetic nephropathy, which has become the leading cause of kidney failure in the United States. Consistently elevated blood sugar levels trigger a series of destructive changes within the delicate filtering units of the kidneys.
High glucose concentrations cause the walls of small blood vessels in the kidneys to thicken and become scarred. These tiny vessels, called glomeruli, normally filter waste products from the blood while retaining essential proteins and nutrients. When damaged by diabetes, they begin leaking protein into the urine while becoming less efficient at removing toxins.
The initial stages of diabetic kidney disease often go unnoticed because symptoms rarely appear until significant damage has occurred. By the time protein appears in urine tests or blood pressure begins rising, substantial kidney function may already be lost. This silent progression makes regular screening essential for anyone living with diabetes.
Advanced diabetic nephropathy can progress to complete kidney failure, requiring dialysis or kidney transplantation to sustain life. The progression from normal kidney function to end-stage kidney disease typically occurs over 10 to 20 years, but the timeline can vary significantly based on blood sugar control and other health factors.
High blood pressure pounds kidneys relentlessly
Hypertension creates a vicious cycle with kidney disease, where high blood pressure damages kidneys while kidney damage further elevates blood pressure. This destructive feedback loop accelerates kidney deterioration and increases cardiovascular risks simultaneously.
Sustained high blood pressure forces blood through kidney vessels with excessive force, gradually damaging the delicate filtering structures. The constant pressure causes scarring and narrowing of blood vessels, reducing the kidneys’ ability to receive adequate blood flow and oxygen.
As kidney function declines, the organs become less capable of regulating fluid balance and blood pressure through normal mechanisms. The kidneys respond by retaining more sodium and water, which increases blood volume and further elevates blood pressure. This creates an escalating cycle that becomes increasingly difficult to control without medical intervention.
Uncontrolled hypertension can progress to malignant hypertension, a medical emergency where blood pressure rises so rapidly that it causes immediate organ damage. When this affects the kidneys, it can cause acute kidney failure that may become permanent if not treated immediately.
Heart disease and kidneys share dangerous connection
The relationship between cardiovascular disease and kidney health represents a complex bidirectional connection where problems in one system inevitably affect the other. This relationship, known as the cardiorenal syndrome, significantly increases mortality risk and complicates treatment strategies.
When the heart fails to pump blood effectively, it reduces blood flow to the kidneys, impairing their ability to filter waste and regulate fluid balance. Simultaneously, kidney disease contributes to cardiovascular problems by disrupting normal blood pressure regulation and promoting inflammation throughout the body.
Chronic kidney disease accelerates the development of atherosclerosis, the buildup of plaque in arteries that leads to heart attacks and strokes. The inflammation and metabolic changes associated with kidney disease create an environment that promotes cardiovascular damage even in younger individuals.
The medications used to treat heart disease can sometimes affect kidney function, while treatments for kidney disease may impact cardiovascular health. This creates complex treatment challenges that require careful coordination between different medical specialists to optimize outcomes for both organ systems.
Metabolic syndrome multiplies kidney threats
Metabolic syndrome, a cluster of conditions including obesity, insulin resistance, high blood pressure, and abnormal cholesterol levels, creates multiple pathways for kidney damage. This syndrome affects nearly 35 percent of American adults and dramatically increases the risk of both diabetes and cardiovascular disease.
Excess abdominal fat produces inflammatory substances that directly damage kidney tissues and promote insulin resistance. The chronic inflammation associated with obesity creates oxidative stress that accelerates kidney aging and reduces the organs’ ability to repair themselves.
Insulin resistance, even before diabetes develops, can impair kidney function by altering normal glucose and fat metabolism within kidney cells. These metabolic changes make kidneys more susceptible to damage from other factors like high blood pressure or toxin exposure.
The combination of multiple metabolic abnormalities creates a synergistic effect where the total kidney damage exceeds what would be expected from any single condition alone. This explains why individuals with metabolic syndrome experience rapid progression of kidney disease once it begins.
Autoimmune conditions attack kidney structures
Various autoimmune diseases can directly target kidney tissues, causing inflammation and scarring that progressively destroys normal kidney function. Lupus nephritis, a kidney complication of systemic lupus erythematosus, affects up to 60 percent of lupus patients and represents one of the most serious manifestations of this autoimmune condition.
In autoimmune kidney disease, the body’s immune system mistakenly attacks normal kidney tissues, creating inflammation that damages filtering units and blood vessels. This immune-mediated damage often occurs in cycles, with periods of active inflammation alternating with relatively stable phases.
Rheumatoid arthritis and other inflammatory conditions can also affect kidney health through chronic inflammation and the medications used for treatment. Some anti-inflammatory drugs commonly used to manage these conditions can reduce kidney function when used long-term or in high doses.
The unpredictable nature of autoimmune diseases makes kidney protection particularly challenging, as disease flares can cause rapid deterioration in kidney function. Regular monitoring and aggressive treatment of autoimmune activity becomes essential for preserving kidney health.
Lifestyle factors accelerate kidney decline
Beyond medical conditions, several lifestyle factors significantly influence the rate of kidney disease progression and the overall risk of developing kidney problems. These modifiable factors often represent the most practical opportunities for kidney protection.
Smoking creates multiple pathways for kidney damage by reducing blood flow to the kidneys, promoting inflammation, and accelerating the progression of underlying conditions like diabetes and hypertension. The toxic chemicals in tobacco smoke directly damage kidney blood vessels and interfere with normal repair mechanisms.
Excessive alcohol consumption can lead to acute kidney injury and chronic kidney disease through its effects on blood pressure, liver function, and overall metabolism. Alcohol also increases the risk of dehydration, which can stress already compromised kidneys.
High sodium intake forces kidneys to work harder to maintain proper fluid balance while contributing to high blood pressure development. The standard American diet contains far more sodium than kidneys can process efficiently, creating unnecessary stress on these vital organs.
Inadequate water intake can concentrate toxins in the kidneys and promote the formation of kidney stones, while excessive water intake can dilute essential electrolytes and strain kidney function. Finding the right balance becomes particularly important for individuals with existing kidney problems.
Early detection saves kidney function
The silent nature of kidney disease makes regular screening essential, particularly for individuals with known risk factors like diabetes, hypertension, or family history of kidney problems. Simple blood and urine tests can detect kidney problems years before symptoms appear.
The estimated glomerular filtration rate, calculated from a basic blood test, provides an accurate measure of kidney function that can track changes over time. Even small decreases in this measurement can indicate significant kidney damage that requires immediate attention.
Urine tests can detect protein leakage, an early sign of kidney damage that often appears before other symptoms develop. The amount of protein in urine correlates with the severity of kidney damage and helps predict future progression.
Blood pressure monitoring becomes particularly important for kidney protection, as even modest elevations can accelerate kidney damage over time. Home blood pressure monitoring allows for better control and earlier detection of hypertension-related kidney problems.
Protection strategies preserve kidney health
Preventing kidney disease requires a comprehensive approach that addresses underlying health conditions while implementing kidney-specific protection strategies. The earlier these measures begin, the more effective they become in preserving long-term kidney function.
Optimal blood sugar control remains the single most important factor in preventing diabetic kidney disease. Maintaining hemoglobin A1C levels below 7 percent significantly reduces the risk of kidney complications while slowing progression in those who already have kidney damage.
Blood pressure control to levels below 130/80 mmHg protects kidneys regardless of the underlying cause of hypertension. This often requires multiple medications and lifestyle modifications, but the kidney protection benefits justify aggressive treatment approaches.
Regular physical activity improves blood sugar control, reduces blood pressure, and helps maintain healthy body weight. Exercise also improves cardiovascular health, which indirectly benefits kidney function through improved circulation and reduced inflammation.
Dietary modifications focused on reducing sodium, processed foods, and excessive protein can reduce kidney workload while supporting overall health. Working with nutrition professionals helps ensure dietary changes support rather than compromise kidney function.
The intricate connections between chronic illnesses and kidney disease underscore the importance of comprehensive healthcare approaches that recognize these relationships. By understanding how conditions like diabetes, hypertension, and heart disease affect kidney health, individuals can work with their healthcare teams to implement protection strategies before irreversible damage occurs. The silent nature of kidney disease makes proactive management essential, as symptoms often don’t appear until significant function has been lost. Through early detection, aggressive treatment of underlying conditions, and lifestyle modifications, it’s possible to preserve kidney health and prevent the devastating consequences of kidney failure.