Ramona Burress, PharmD, is the Head of Patient Engagement and Insights within the Center for Health Equity and Patient Affairs at Takeda Pharmaceuticals. In this role, she works with various Takeda teams to oversee the design and integration of patient engagement across the clinical continuum, integrating invaluable patient insights to inform each stage of the drug development lifecycle. This work enables Takeda to be even better positioned to bring innovative medicines to more patients in more communities and to co-create health-promoting environments where everyone has the access and resources they need to thrive and reach their full health potential.
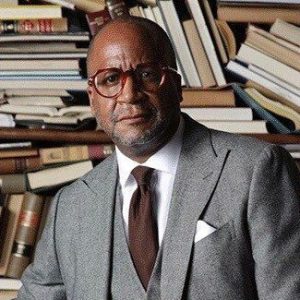
She visited with rolling out a few years ago to talk about surviving breast cancer. Now, she follows up with more about self-care as she speaks to the renowned publisher Munson Steed in the first part of a two-part interview.
[Editor’s note: This is an extended transcription. Some errors may occur.]
Munson Steed: Hey, ladies and gentlemen, this is Munson Steed, and we are literally on Health IQ. It’s where we work diligently, and I would say, even honestly, to help make that distance between our IQ going up and the community being able to expand their intelligence about how important health is each and every day. And that you are a healer just in yourself, having the faith and understanding that you’ve gotta have some relationship with the health system and your body and health practitioners all around you.
So, I am proud to say that I am hanging out with my dear sister here on Health IQ, Ramona Burress. Let me know, and if you would just share what your day job is, and how it is, and then we’ll talk about the intersection of where health became a primary consideration that others can find inspiration in.
Ramona Burress: Oh, yes, definitely. Thank you, Munson. First of all, for having me be a part of this platform to talk about my experience personally as well as professionally, and how they really do blend together. My day job: I am an executive at a pharmaceutical company, and I oversee our approach to integrating health equity into how we do drug development. Simply put, how do we understand more so from patients who are our customers and their caregivers, their loved ones, about the medications that we are researching, to see if they have a true impact from a quality of life perspective, but also from a clinical perspective on outcomes of folks who are living with many different diseases.
And basically, I see it [as] humanizing drug development. And it’s a really rich and exciting job because inherently, what comes with that is diversifying the population of folks that we touch, either through clinical trials, access, or just even when medications are approved on the market.
How do we make sure that all communities globally have access to those medications? But that starts from the beginning, right? Really understanding, hearing from the lips of patients directly and folks have been to this patient ecosystem, so their providers, their loved ones, their caregivers, about what are some of the gaps in their current therapy, and just who they are as a whole person who’s living with a certain condition. And that really does stem from my personal experience as a metastatic breast cancer patient but also my years of direct clinician experience being a pharmacist.
MS: You know, for the young people out there trying to figure out how soon should they tap into understanding their health? And how soon should they be going to annual checkups and understanding family history? When should we start this conversation as a family unit, no matter what the makeup is on health?
RB: I love that! As early as possible, I think around a dinner table is probably key. I know so many of us have households where, you know, you’ve got 2 parents working, or maybe it’s a single-parent household, and there’s 5 different TVs in the house, and we’re all on our phones 24/7. But I think returning to that sense of normalcy of gathering around a dinner table, even if it’s once a day at grandmother’s house, big mama’s house. Even if it’s just those Thanksgiving and holiday, you know, check-ins. Easter is coming up upon us, but really having honest conversations about our family history.
And really, that is very much so parallel to just talking about our medical history because if you think about, you know, conversations and what we have, what now is, we have about our own families. I know that you know my Grandmama died from sugar, but what does that mean, you know? Did she have diabetes? Probably yes, check the box. And did she have cardiac complications from uncontrolled diabetes that led her to having a stroke? But better understanding, you know, in those informal settings where folks are just gathering, you know, just to talk about. Hey, these are some of the challenges our elders are facing. These are some of the current challenges I, you know, I’m facing in my middle age.
But then, you know, also, including the kids, the teenagers in that space. And I think that’s important too, when you think about, like depression coming out of Covid, and everyone was impacted financially or with, you know, having this direct death experience in their faces. We got our young kids who have these gaps in education. And now, you know, matriculation is getting harder, now they’re aging. So it’s real out here, right? Life is “lifing”. Taraji told us, you know, “the money, the math ain’t mathing, life is lifing”. So, thinking about just all these potential threats to our families that do also, you know, trickle down into how they approach their health. I think it’s just part of that normal conversation we need to bring back to the table.
MS: When you think about a person like yourself, and you decide that, being a pharmacist to being a part of that group, that elite group, it finds itself in either Pharma or even providing health and being an advocate at it. Why should our community also lean into both the pharmaceutical industry and participating, you know, in the healthcare industry?
RB: I love it. That’s a great question. We need to be at the table when decisions are being made. There are great organizations like I am able here in Chicago and some others where they really push on. Those of us who are credentialed, who are clinicians to go back into the schools, go back into the mentorship. We need to start early there to let our kids know that. Hey? This is possible. You could be a doctor, you could be a nurse. You could be a nurse practitioner, you could be an anesthesiology technician. But there are so many different pathways outside of a, what I think is introduced to us, you know when we’re in grammar school like, [woo] I wanna be a lawyer. I wanna be so-and-so but you know, really, we’ve learned that when you see it you believe it.
When you see it, it becomes a reality, and so the onus is on us. Those of us who are out there practicing, you know, have these credentials, have these fancy jobs. Take it back to the beginning, so that we start to encourage this pipeline because it’s all about that knowledge, that self-awareness, that self-determination, that then starts to open up doors for students, as they age through the system. And where to, we also have to, you know, bring in opportunities for fellowship, internship opportunities, or volunteering or shadowing a day off so and so. So I think that’s you know, one way that we introduce these opportunities by direct practical experience.
But then, too, just making sure that we really look at the education system and making sure that you know whether it’s a university setting, that there are adequate opportunities for folks to lean into their interest, whether it is that, her terminal degree, or whether it’s something else. So I think that’s something that those of us now who are sending these seats need to make sure that that’s continuing for this pipeline of young kids who are coming behind us.
MS: You talk also about you know, how important it is for us to think about clinical trials. It’s someplace that is not often talked about, in people of color. And so, I’d like for you to talk about, one, the importance of clinical trials, but what happens if we don’t participate in clinical trials?
RB: That’s another good question. So, research has a complicated history in our communities. We’ve got, you know, examples such as Tuskegee. You know, we hear about Henrietta Lex. But there are benchmarks that have changed in research, where we’re protecting the rights of those who are coming in as participants. So, there’s internal review boards that look at, you know, proposed protocols for research. There’s all these checks and balances that weren’t there before. That now, you know, research is being conducted safely.
And so, as we move into this age of like personalized medicine you hear so much about, you know, cancer medications that go after specific protein expressions. We’ve gone away from the old, you know, again, grandmama, who had diabetes and high blood pressure. She was on a water pill. Those days are gone. You know. A lot of our medication therapies are very much so targeted towards different elements of disease that are newer, and they’re not the same universally. So you may see a protein that’s overexpressed and you know, people with ancestry, you know, that lean towards Africa, versus other folks who may be from other parts of the world. And so the more that we are present in this, you know, space as we get to learn more about medications which will be the trials, that’s when we know that these medications are truly gonna be beneficial for our community.
So just, I really like to put out there that, you know, things have changed. People are protected when they come into a clinical trial setting. You know, it’s definitely an intimate conversation that one should have with your provider. If you see a doctor, if you see a nurse practitioner, talk to them, explore some opportunities for participating in research. It’s not always the medicine of last resort, right? But it could be immediate access to something that’s new and groundbreaking, maybe, that you have to take less often if it’s a pill, or maybe a pill with fewer side effects, but the more that we’re counted in this rich scientific data that comes out of clinical trials, the better we are positioned when these drugs are approved and our doctors are prescribing them. So that’s, I think, is the important piece that we just need to be in many different phases of this direct development life cycle process, but definitely, the clinical trials, so that you know people know how these medicines will work and folks that look like us.
MS: Thank you for that, moving just closer and more personal for women. Women’s health, we are now, you’re not the superhero whose cape can cover everybody and expose yourself trying to protect everybody. What? And how should women take their agency back for giving themselves to the world? Having a demand, not even in a freeway, dramatically. Both the obviously the way we came here, and then the way the dynamics of both male-dominated society is perpetuated, a fraudulent relationship that really strains both mothers, women, caretakers to the nth degree, when you’re black. What says thee to the women about? Take your agency of self-care, self-protection, self-love… Self-care has to come first…
RB: Yeah, that’s a good question. I think it’s about looking at the bigger picture. I think it’s about first being okay with being selfish. But so often, you know, that selfishness that we engage or approach as black women could be in buying that purse that I work damn hard on my job. So, I deserve this $5,000 purse or going to get our hair done every two weeks. But what does all of that, or any of that, mean if we’re not healthy? You know, because that selfishness means that we’re taking ourselves away from our family. That can be our kids, spouses, extended family, you know, if you’re a caregiver to a parent all these different, you know, hats that we wear, but they all come at a toll.
And so again, as we kind of look at okay, selfishly, I’m gonna buy a purse cause I deserve it. I work hard. But let’s take a step back and let’s look at you know. How’s your blood pressure doing? Again, knowing your family history, knowing that, you know, your mom is dealing with something, or your aunt is dealing with something. How do we make sure that you’re good, right? And just going in and just having those well checks with the provider, I think is important, but I think that means telling everybody, you know, get off me for a second, so I can, you know, go see my doctor. That could be work, taking a day off of work to go to the doctor. That could be, you know, sometimes transportation, copay, all these different things.
But setting aside, you know, those resources you, you know, you need just to go in and be seen by someone. So taking that definition of selfish, taking that definition of, you know, we gotta do everything for everyone else and just position it back to ourselves. There’s always this adage about, you know, put your mask on first when you’re on the airplane, like, if the plane starts to go down. I think that’s definitely, as black women and women of color. You know, we really need to revisit that, make sure that we’re showing up whole, because if we’re fractured, or if we’re half, you know, empty cup, we have less to offer, and those who are dependent on us, again whether it’s family, career, what have you. So I think that’s just something that we just need to keep championing.
And you know, and as I’m telling this to your audience, I have to remind myself of the same thing. I have two beautiful kids who just graduated high school, and now they’re in college, and last year was all about them, them, them, them. And then, you know, I was like, Oh, I can’t breathe. I’m like, Oh, this must be that COVID. No, girl, it’s your heart, right? But it really took me to, like, have issues breathing, then I’m like, “Let me go see my doctor.” And sure enough, you know, I had to be evaluated for some other things.
So, to all the women who are out there watching, let’s not drive ourselves to the point of exhaustion. Let’s not drive ourselves to the point that we’re experiencing symptoms. But really, take that time to carve out our schedule for self, you know. Maybe, replace that hair appointment is coming up next week, and just go do that check in with your Gyne, and then the next one. Do your check in with your primary care. But I think that’s the message that I want, you know, the audience to hear.
MS: You know that was a beautiful sharing, but it’s Telltale signs, listening to the body. What have you learned about listening to the body that really saved your life? And has saved you from more complications in your health by listening to your body and your feelings.
RB: Hmm! That is such a good one. So, in my day job, you know, it’s centered around patient engagement. And really, I’m pushing for us to recognize patients or people as the experts of their own body, as the experts of their own health journey. And whether it’s me talking to a group of women who are breast cancer survivors. It’s about, hey, make sure your voice is being heard when you’re in a room with that doctor. You may have symptoms, you may have, you know, some side effects with some medications. Keep saying it until someone hears you, and if that person doesn’t hear you. You know what? Try to find a new doctor, or try to find someone else who will listen to you.
So I think it’s just elevating that piece of it and recognizing that, you know when something doesn’t feel right. And sometimes, even when you are engaged in routine care, something may get missed. Because the lab is not all for, or there’s no obvious signs. But the minute a woman knows something is wrong with your body, whether it’s your cycle, whether it’s, you know, a lump in your breast, or just headaches that are, you know, abnormal.
You’re taking too much Excedrin, right or too much headache medication. Keep an eye on that, and report that, you know, be willing to… We advocate so much for other folks, our parents, you know, our kids, and you know, the community, do the same for self. If something doesn’t, you know, feel right, go get checked, go get seen. So you don’t have to be rushed to an ER, you know, later on. But just be upfront like you know what this isn’t feel right. Let me check in. Let me have my doctor check this out. And then in those phases, just keep saying, Okay, I know I talked to you about this 2 months ago, but it’s still happening. I know you gave me this medication, you know. But this ain’t it. Let’s try something else.