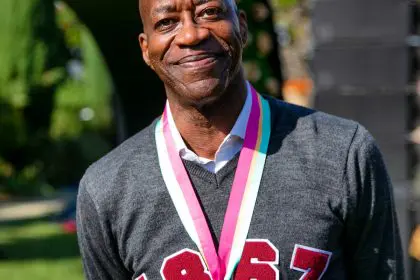
Dr. B.K. Edmond is a board-certified anesthesiologist with more than 25 years in the field. He is a graduate of Morehouse College in Atlanta, Harvard Medical School ’90, and Harvard’s Brigham and Women’s Anesthesiology Residency. He is a former military physician and has worked at Walter Reed National Military Medical Center since 1994, where he is one of their master clinicians. He has been on staff at Johns Hopkins Anesthesia and Critical Care since 2009, where he works regularly in the Weinberg Cancer Center.
Dr. Edmond has been actively engaged in mentoring and assisting underrepresented students interested in health professions over the course of his career. Over the past eight years, his roles have increased as he led the Morehouse College Office of Health Professions Alumni group. He has hosted numerous events over the years that focused on mentoring for students interested in health science. His most recent event was in Atlanta during the 2019 Super Bowl Weekend. He brought together over 250 pre-health students from over 10 institutions for a mentoring breakfast. This event featured over 200 physician/dentist mentors. (www.DrsWeCantWait.org)
He is a member of the National Association of Advisors for the Health Professions (NAAHP) and is one of the physician speakers featured on the Black Men in White Coats podcast. His motto is, “The race is not to the swift nor to the strong, but to him that endures to end.” He is on the Board for PAUSE and Pre-Med Solutions, two Atlanta-based nonprofits that work to increase the minority presence in medicine and dentistry.
Dr. Edmond also serves on the board of the DreamHouse Make-A-Difference Foundation, a nonprofit organization that directs opportunities to the youth in Atlanta. For more details, visit www.dreamhousefoundation.org.
Dr. Edmond’s Website: www.TheBEdmondProject.com.
He took time to discuss some weighty maternity issues with Munson Steed, publisher, and CEO of rolling out.
[Editor’s note: This is an extended transcription. Some errors may occur.
Munson Steed: Hey, everybody! This is Munson Steed. Welcome to another edition of Health IQ. Where we bring you the biggest and the baddest, and probably some of the best. Not probably, the best, power of healing, power of health, and reducing the difference between health disparities and the love and care that we think everybody deserves just as humans. The distance for those who are there. This is a special moment for me, for obviously, being a proud Morehouse man.
My dear brothers and sisters over at Spelman, who are really making a difference in this community, and the healing has come together with something special. Dr. B.K. Edmond. Come on off mute, participate in this conversation, and tell us: What is the movement that we all need to keep our eyes on? Because we’re not making progress in our IQ or at least the service IQ, That we’re delivering and need to be demanding is not being met, as it relates to maternal mortality for black and brown women.
Statistics paint a grim picture
Dr. B.K. Edmond: Gotcha. Well, in terms of maternal mortality for black and brown women right now, probably within the past, like 4 or 5 years, you’ve seen people start to send up these flares, to raise awareness of the crisis. Saying that black women are dying at 3 times normal. Black women are dying at 3 times the normal. The reason for that is because, when you look at what happened, you actually had the statistics start to be generated on Black maternal mortality. But you actually up until about really 4 or 5 years ago, it was tough to get quality statistics on what was happening.
Now, let me tell you what those statistics showed about America, and I’m gonna make it simple for your listening audience. We’ll do it by the numbers. No. 1, in the past 20 years the incidents for death and injury during pregnancy for all women in America — that’s all women, Black, White, Jew, Gentile — have doubled. Okay, so, in the past 20 years the incidence of death for mothers, not Black mothers, has doubled.
The second number I try to teach people is three, and that is that black women die at three times the normal rate during pregnancy.
The third number I try to get people to understand is 60, because 60% of the deaths occur after that child is born. So, it’s not the 9 months leading up to the delivery or the good times for those 9 months after conception. It’s actually about 6 weeks after the delivery that most of those mothers fall off and get injured, and that’s the Red Zone that we’re trying to really get people to focus on. And the last number, and this is the one that’s the most sobering is 80, and a recent study came out to show that 80% of the deaths and injuries for mothers in America are 100% avoidable.
So, you have needless people being injured. Eighty percent of those, so literally, 8 out of the 10 times a mother dies or mother gets injured, there’s something in her care that could have saved her life that was missed. So, with those numbers alone, it raises the urgency. There’s only one other number that I’ll mention, Munson. Remember I told you that in America the incidence of death was going up and had doubled or increased by a hundred percent or doubled? In the rest of the world, it has decreased by almost 40%. So the rest of the world is over the past 20 years getting better, in terms of survival for mothers and less injury during delivery.
U.S. statistics trending the wrong way
The United States has been identified by the World Health Organization as one of about seven or eight countries that’s going in the wrong way. And we’re going in the wrong way and between like, I think it was 2021 to 2022 or 2021, in one year it increased by 40%. So the whole key is, we’re going the wrong way faster. So that’s the urgency component that really made me move on this issue as a provider.
That’s really, and if those numbers don’t make you … understand that this is an issue, there’s nothing we can do. But can I tell you one other issue, one other just number that takes it home. In the country of Finland, in certain European countries, the death rate is 20% less than America. Literally, you may have one to two women die for a 100,000; in America we’re 20 to 30. So, the key is, this problem has been fixed in other countries and we’ve actually made conscious decisions in healthcare, and how we apply health in America to cause problems.
MS: When you think about that, let’s go to six weeks post-conception. If you’re a family member and your sister or your wife or your cousin has just had a child, what should we be aware of for the next six weeks?
BK: Excellent question. And what you’re asking, Munson, is actually the entire focus of what the CDC “Hear Her” campaign is about. The CDC created an entire campaign that’s designed to train the Black family, Black community to recognize a mother in distress. So there’s symptoms that happen that they can say that a mother’s having problems and the symptoms quite frankly can be broken down. Either they have to deal with blood pressure. They usually have to deal with some type of bleeding. They have to deal with some type of, usually infection, and then there’s some other components that believe it or not, like depression. And psychological issues that can cause problems.
The reality is, there’s a sheet that has all of the symptoms on it but I sum them up into those groups. One is high blood pressure and high blood pressure if it occurs at any time during pregnancy is the issue, because the hormones that the mother has in her body normally drops the mother’s blood pressure. But what happens is as that child develops at about maybe 30 or something, 30, 32 weeks into this thing, what happens is the placenta, which is the part that connects the part that kind of like that connects to the mother’s blood circulation.
Well, sometimes, if that placenta is not working correctly. The placenta will start putting out hormones that raise the blood pressure of the mother, so that it can drive more nutrients into the child. So, if that placenta feels like it’s not getting enough nutrients sometimes, or for some other reason. Some people think it’s genetics and other things. What happens is, that placenta, when it gets big enough, will start releasing a hormone that causes the blood pressure to go up in the mother. The problem is the mother’s systems are not designed to handle that.
So what happens is the women can have strokes, they can get seizures, they can get kidney failure. They can develop something that’s called Help Syndrome, where you actually have your liver get congested. The key is blood pressure that’s normal in you, that it’s not normal. But you may say, if someone says, your blood pressure, your top number on your blood pressure is 150 and your bottom number’s 90. They’re not gonna send you directly to the hospital, Munson. They’re gonna tell you, “Come see me in a clinic, and we’ll put you on some medicine, and we’ll see how it works after a couple of weeks and come back.”
If a mother has a blood pressure of 150 over 90, she’s actually knocking on the door of a medical crisis. So, she will actually need to be admitted to the hospital, have a IV started and put on special medicine in order to control that mother’s blood pressure. The problem is, Munson, is it doesn’t just occur in the nine months before. It occurs in that six weeks after, and it can actually occur up to a year out. You can have some symptoms from the mother. So, when you ask the symptoms, the different categories, things we look at — headaches, swollen legs, swollen feet, shortness of breath, the pain in your abdomen, and this is at any time during the delivery. Undue vomiting, that’s not necessarily. And so there’s those symptoms but they have an easy way to teach you that on the “Hear Her” site for the CDC.
MS: We’ll share some facts here for you there. But I think it really causes accountability when I think of it as a media person. And I think that, how do we have accountability partners for a year post?
BK: You’re 100% on that and that ties into one of the major things. One of the major contributors or things that have been done to actually increase and improve outcomes from mothers. And that is actually, the use of doulas. Doulas are women who specialize in walking mothers through the delivery process, meaning that when they get pregnant. They team up with the mother, and they coach that mother on what it means to take care of the child. How to take care of themselves in the nine months.
Black women tend not to be heard
But after that delivery, the doulas [are] actually trained already to recognize those symptoms, but more importantly, they serve as an advocate for the mother. So that, if that mother has a problem and has to engage the healthcare system. Somebody has her back and makes sure that she’s heard. And believe it or not, with the doulas, you have an improved outcome, because you have an advocate associated with it. As far as carrying it out for a year or so, that’s fine, that that sounds great as well. But the reality is, Munson, one of the main problems here is that mothers are not being heard.
Black mothers are not being heard, when they engage the healthcare system. And that’s why they form the “Hear Her” site. I mean, the classic example is Serena Williams when Serena Williams had her check out a day or 2 afterwards. She was having a clot. She felt like she had a clot that traveled to her lungs, and that’s called a pulmonary embolism. Well, unfortunately, Serena had had one of those earlier in her life, so when she reported to the nurses station that she was short of breath, and felt like she did when she had a pulmonary embolism.
The nurses said, “Oh, that’s okay. It’s just you’re nervous. It’s okay.” Now this is right after she had a child, and she told them, “No, I feel like I felt when I had the clot in my lungs that nearly killed me.” And they said, “We understand you’re anxious” and they basically blew up. It wasn’t until she got her own team involved, that she was actually heard by the system. And so the reality is, one of the major problems is not being heard. The Black women are saying the right things. They’re going into an institution and an establishment that doesn’t have the ability to hear a Black woman, a Black woman’s cry.
And so, that’s why you have the “Hear Her” component, which is designed to teach families the symptoms, but also teach the families how to engage in the healthcare system. That’s why the next title of my book is called The Quote Makers: The Art of Hearing a Black Mother’s Cry. The problem is not that we don’t have the equipment. The problem is our Black mothers and our Black women are not being heard. So you have to have an advocate involved if you engage the healthcare system when you’re pregnant.
MS: Right. And what your brother is working for our community to hear is that we want that woman, that sister, that mother to have accountability partners who can take the role to allow the system to hear her cry.
BK: Right.
MS: And not have just even one, ’cause we’ve got to check that group. So let’s all create a system of check-ins with our sisters and mothers. So we’ll be happy just as many people as we have at the baby shower, for those 6 weeks to a year. Be present, listen, and allow them all to celebrate and take a different responsibility. Post-childbirth.
BK: Absolutely and post-childbirth Munson and because 60% of the deaths occur post-childbirth. And that’s when people are taking their eyes off of the Black mothers and off of the mothers. And we really did, back in the day, we didn’t have to worry about this, because whenever somebody got pregnant, there was auntie, or mother, or a grandmother that would come and sit with that woman about, a couple of weeks before the pregnancy, and for six weeks after the pregnancy.
And it was that matriarch, that mother, that was responsible for making sure that, “Hey! Something’s not going right.” She’s seen it a hundred times so she can raise the issue, and she’ll advocate for it. But the reality is that our black mothers need an advocate and everyone always tries to blame the victim. But one of the No. 1 demographics that’s having problems, that has one of the worst outcomes is the college-educated black woman. And they actually have studies now to show that a college-educated black woman has a much worse outcome than a high school dropout who’s Caucasian.
So, you have intelligent women telling the system what they need and the system’s not hearing it. So, the remedy has actually been put in place in some institutions. One of the institutions where I work actually instituted a policy, that if a woman who’s pregnant or has been pregnant recently, comes in the door to an urgent care or emergency room, they have to be seen by an obstetrician or a fellow within 45 minutes to an hour of hitting the door. That’s the policy. So, in other words, by having a blanket policy like that, you don’t have to worry about is it a Black woman? Is it an Asian woman? Is it a white woman? The policy is, all mothers get cared but in order to get that policy implemented, there needed to be advocates. And that’s where your listeners come in to the situation and stuff. Each one of you, once you get educated on this, you’re gonna have to be an advocate for the people, for the mothers in your family.
MS: Great. Well, thank you for coming on Health IQ and giving us this vision for ourselves and for our dear sisters. Obviously.
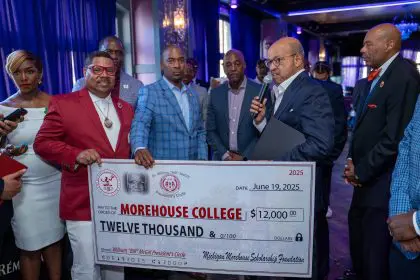
BK: Can I ask you one quick invitation and stuff on Saturday? This coming Saturday at Clark AU, we have a panel of experts in maternal fetal health.. We have an expert from the CDC. We have an OBGYN doctor from Morehouse, from Spelman, and we also have one of the new directors of research for the Maternal Health Center. That’s run by Emory and Morehouse School of Medicine. It’s a live feed. It’s free of charge. When you sign on, we’re going to give away $300 to somebody who signs on to it. And the reality is our job over that hour, and it’s from 9 a.m. Eastern time to 10. We’re not gonna run long.
We want you to be able to sit down with a cup of coffee. Get your hands around this issue and be educated enough so that you can start standing in the gap for your family, and that goes for the men and the women, because remember, if the child passes away, the daddy has to take care. And every birthing mother has a daddy, who’s part of her support system. And so we invite you to come on out and we’ll have the list. We’ll post up the registration site there, Munson. Thank you so much for having me.
MS: Thank you, Dr. Edmond, for continuing to push this issue forward. Maternal mortality is an issue for women, but Black women in particular.
Everyone, be sure that you “hear her”; look on CDC.gov to get more information today on “Hear Her.” Share it on your page. This is an important fact that our women, Black women, are suffering at an inordinate proportion that needs to be heard and dealt with today. So if you love somebody, show them by sharing with the entire family, with all of your Facebook friends, to all of your rolling out family. The very essence of what “Hear Her” and what Dr. B.K. Edmond has to say about being able to put a quilt, the warmth and intelligence, and help around our community. I’m Munson Steed, here for more Health IQ with Dr. B.K. Edmond.