Dr. Mary Branch, a cardiologist, is a fourth-generation African American physician who has broken new ground in her journey and unwavering commitment to cardiovascular health. Her story is a compelling testament to resilience, determination, and pursuing one’s dreams.
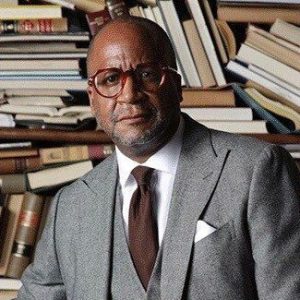
Dr. Branch’s remarkable journey from her roots in Cleveland, Ohio, to becoming the first African American female to join the Cardiovascular Disease fellowship at the Wake Forest Baptist Medical Center is a narrative of willpower and triumph. Her educational achievements and perseverance through setbacks exemplify her dedication to serving others and transforming obstacles into opportunities. She spoke with rolling out publisher and CEO Munson Steed about her journey.
[Editor’s note: This is an extended transcription. Some errors may occur.]
Munson Steed: Hey, everybody, this is Munson Steed! Welcome to another edition of Health IQ, where we find the biggest, brightest, boldest individuals who genuinely provide insight and information on how we can increase our health IQ and save our lives simultaneously. I am most proud to introduce my dear sister, Doctor Mary Branch, who truly is a servant. As a medical doctor, she is here for us. How are you?
Dr. Mary Branch: I’m doing well. Thank you for that introduction.
MS: Well, let’s get right to it. There, you decide to be a cardiologist. How did [you arrive at] cardiology of all the practices?
MB: Right.
MS: What happened?
MB: Right, exactly. There are many different options in medicine. I chose cardiology [as my first choice], and I’ve been very privileged. I’m a fourth-generation African American physician, so I’ve been exposed to medicine. My family’s intent has [always] been to serve the community, and they chose medicine as a way to do that for four generations. My mom was in infectious disease, [and I thought I didn’t want to] do that. I just got queasy. I [didn’t] know how she could eat and see all these infections, so that wasn’t for me.
But she allowed me to [do] some shadowing – [where] you can [see] what different doctors do – when I was in college. I shadowed different types of doctors [from infectious disease to emergency medicine to cardiology, which is when a light bulb went off]. It was just a spark, [an instant connection with being interested in the field]. You [do] many different things in cardiology, [such as interventions, stress tests, imaging, and readings]. That [fit] my personality because I knew I didn’t want to do one thing. I want to do [many] different things, but they [are all] tied together.
At the same time, there was a film called “Something the Lord Made” about a researcher, Vivian Thomas, and how she was working on a procedure for a congenital heart disease defect. Those two things [coincided, and it seemed like a sign that this was a journey I would go on similar to Vivian Thomas, and also] this passion that I instantly developed.
Then, my stepdad [passed out while driving] and almost passed away. Thankfully, he got bypass surgery, [with] which he was able to live for a long time. So, certainly, heart disease plagues the African American community, [and I found a way to serve in that capacity to continue] my family’s legacy, [and] here I am.
MS: It brings me to the point. We think about heart attacks, and we might think of men. However, heart attacks affect women in large numbers. And what would you say if you were speaking to all the black women in the world right now about their heart care?
MB: Sure. Your heart care is extraordinarily important. For one, unfortunately, we’re seeing a lot of cardiovascular disease risk factors in younger folks. [I want to emphasize] where we see some of the inequity with care [as we’re getting risk factors and issues related to heart disease in our thirties and forties that folks of other races may be getting later on in their fifties or sixties]. So, it’s important [to] establish with a primary care doctor and know [your metrics]. Forty should be [the oldest] that you establish [care].
But really, [considering it’s Black Maternal Health Week, after you deliver, especially if you have any issues giving birth, know what your metrics are, what your blood pressure is, and understand that a blood pressure of roughly 130 over 80 is expected. Screen for diabetes. Know your family’s history. Does everyone get a heart attack when they’re in their fifties? You want to know that so you can talk to your physician about that and look for a particular screen] you might need.
So for African American women, I would say, if you’re thinking, “Oh, I can wait until I’m 60 before I see a doctor. Wait till I have symptoms.” You really wanna act from a preventative strategy. So, start young, again, if you’re thinking about having children around that time. But definitely before 40, and know your metrics and know what’s normal and really be diligent about keeping your weight in a healthy range and your blood pressure in a healthy range. But again, I just emphasize having a relationship with healthcare early is extraordinarily important for prevention of heart disease and stroke.
MS: You truly are very kind. I can see people coming in, but let’s just be a little bit more candid and honest with people as it relates to the metric. The [risk] if you wait till 40, and you are smoking at 25. You see a lot more vaping. What would you say to young sisters who are vaping and might be overweight that they’re not thinking about? Or sisters that are vaping and literally have very stressful jobs or not knowing their blood pressure and vaping?
MB: Right. Vaping, I don’t know if we have enough data at this point to look at sort of the cardiovascular use risk factors. Certainly, you can get sort of this interstitial lung disorder. So, it’s still dangerous. It’s not a safe thing to do. [There are] still risks, and if anything happens to the lungs, that’s gonna impact the heart because the lungs and the heart are connected. So anything that you do to your lungs is gonna impact your heart in a negative way.
In terms of, if you’re vaping your stress and overweight, I mean, these are things to one, name it and just say I am overweight. I’m doing things that aren’t healthy. I think a lot of times there is a little bit of denial about our lifestyle and kind of lack of that sort of hard truth that what we’re doing is not healthy. And we’re challenged with accountability. Certainly, there are other factors that impact our health, our jobs, and systemic racism. Those are definitely there. But there are a lot of things that we can do as individuals to change and prevent a lot of these sorts of big conditions. So.
MS: I’m clearly there and wanna push continuously because I don’t get to talk to cardiologists as often as I’d like. But smoking, if you’re smoking and your heart, what does smoking do? To play a role where in the state of what you see or what you’ve experienced.
MB: Right. So, smoking is the worst thing you can do for your health. Smoking contributes to heart attack, which can lead to heart failure. Smoking can contribute to stroke and smoking just overall, it can lead to peripheral artery disease. So, disease in your extremities, and some people require amputations. So, their legs are being cut off because those vessels are damaged. So, smoking is certainly the worst thing you can do for your health and, of course, your lungs. You can develop COPD, and that can impact the right side of your heart. And so, we could be at risk of cancer, and cancer can increase your risk of heart disease.
So, smoking is certainly the worst thing you can do for your health. If there’s anything you can stop if you’re doing, I would say to stop smoking.
MS: Super. Now, I want to push on. Not that you’re not on top of the world, but let’s talk about being overweight in your heart. What is the impact of being overweight 20 pounds and your heart?
MB: Right. So, being overweight 20 pounds, it’s more about your BMI, your waist circumference. So if your BMI is, say, over 30, if you have a small weight, you’re over 20 pounds, that’s okay. But if your BMI’s over 30, that’s when you’re getting into a range that is more problematic. There are several things that are problematic with obesity. One is the rate of heart failure. So, your heart pumping function can stop working effectively. That’s something that’s lifelong. It’s not just one treatment, and it’s done. So. My mom’s in infectious disease. You get an infection, you treat it, and then it’s over.
But with heart disease, this is what you have for life. So, if you are overweight and you develop heart failure. That’s something you have to live with. Obesity is also a challenge because if you’re very obese, the testing can be challenging as well. We may not be able to get a good echocardiogram on you or get an appropriate stress test. So, it’s hard to detect whether you have heart disease if you are very obese. So, not only are you at risk for heart disease, but it’s also hard to sort of assess for problems.
Or if you’re short of breath, [is that because you’re overweight] or because you have heart disease? So, it’s hard to differentiate between just the chronic problems of being obese and what’s actually putting you at risk for a heart attack or heart failure. So, it’s definitely something that’s pervasive and needs to be addressed.
MS: And lastly, before we go into maternal mortality, the very role that stroke plays in the lives of black women and their hearts.
MB: The role that stroke plays? Yeah, so the risk of stroke and the risk of heart disease are tied together. We talked about high blood pressure. We talked about smoking. So, if you’ve had a stroke, it’s possible that you also have risk factors for a heart attack. So, that’s one. Second, in terms of association with your heart and stroke, you could potentially have a heart rhythm disorder called atrial fibrillation.
So, things that correlate with that again are obesity, sleep apnea, and thyroid disease. And if you’re feeling a racing heart rate consistently, you want to get that checked out, just to make sure, especially if you’re over 60, if you have something called atrial fibrillation, to know what your risks are for stroke. So, certainly, those two entities are tied, and those risk factors are tied. So again, it’s all about prevention for both.
MS: Lastly, when you think about the very position that women are in very stressful positions. And we were saying, start a relationship. What are the values of actually starting a relationship with the physician earlier? You know, in your thirties? What do you learn? What are the possibilities? What are your insights? On, why would you suggest, just in general, if you’re black, establish a relationship with the healthcare provider that you trust?
MB: Sure. So, just know of the theme of Black Maternal Health Week. Again, if you start in your thirties. One, you know what your metrics are. You know how healthy you are before you get into a pregnancy and you just start to establish a relationship. So, you’re working with someone who knows you, and you’re working on treating some of these risk factors for heart disease like high blood pressure and diabetes. You need that consistent relationship to see how well you’re doing. If you just see them one time or you wait too late, then these diseases can wreak havoc, and then you can develop your strokes. You can end up on dialysis or have heart failure.
But if you develop this relationship early, then you have somebody that knows you. So, if you’re in the hospital and you’re pregnant, you’re short of breath, and they can contact your primary to say, Hey, I know this person. These are not her typical symptoms. This is different, and so that might raise some red flags that you say. Look, I have an established relationship, and this hasn’t been an issue for me. Now it’s new. So that’s very helpful. If you have somebody sort of in your corner as your advocate continuously.
One is to ensure that you’re being diagnosed appropriately throughout your care, whether it be pregnancy or just in general. Two is to have somebody checking on your metrics and ensuring that they’re trying to prevent heart failure, stroke, etc. So, it’s extremely important to establish that relationship early, and then you just have someone to go to when you have these questions. That’s extraordinarily important.
MS: So, for all our moms, that literally maternal mortality rates for our black women are not what we’d like them to be.
MB: All right.
MS: It doesn’t appear that most black women are heard as they are. Advocating for care but blood pressure, and you being a cardiologist. It can start before the baby is delivered, and it can persist after the baby is delivered. What do women really need to know and to share in this six weeks after and any time their blood pressure has been diagnosed as high or having an impact on their pregnancy or post-pregnancy?
MB: So, having your blood pressure high during pregnancy. One, you wanna know what medications you’re on. How well your blood pressure is doing throughout the pregnancy? As well, Is this medication safe for pregnancy? And can you breastfeed with the medications that are prescribed? If it’s prescribed by someone that you don’t know, you wanna make sure that you let them know that you are pregnant and that they need to make sure that the medication is safe during pregnancy.
After pregnancy, if you develop something called preeclampsia, where you have to deliver because your blood pressure is too high. Preeclampsia can actually increase your risk for cardiovascular disease, from what the data has shown. So, if you did have preeclampsia during your pregnancy, let’s say your blood pressure does come down. It’s still important to follow up with a physician. And we actually have cardiologists that are specifically focused on women. They have sort of an Ob center cardiology group for women.
So, you can ask your primary to say that you would like to follow this sort of cardiology group that’s focused on women, to help with managing your blood pressure after you give birth. So, what I really wanna emphasize is that if you have these issues during pregnancy, they may stick with you long-term and can increase your risk for heart disease. So, it’s really important that you try to establish with. You can ask and request for a cardiologist that focuses on women to work with your blood pressure moving forward, to help protect from some of these. Like I said, heart failure, stroke.
MS: What other insights would you like to share about maternal mortality? And for all those women who are out there advocating so that they are heard.
MB: Right. A lot of women, when you hear their stories, you learn that they just didn’t feel heard. Serena Williams went in and said she was short of breath, and she wasn’t taken seriously till later on, and she had a pulmonary embolism. So, if Serena Williams is having trouble being heard, then the rest of us certainly will be as well. And even as a physician, when I came in. One, I showed up a little bit later because my mother told me a lot of times. They turn African American women away when they’re in labor. They don’t believe them. So, I ended up showing up later.
Didn’t feel like the treatment was the best going in, and not until I kind of said, “Oh, I’m a physician,” that things changed a little bit. But that’s really problematic. I shouldn’t have had to do that, and I really understand what it’s like on the other side. It’s very scary. So, what I would recommend is just having an advocate with you. If you have anybody in the family who is in healthcare at all having their contact information, so that if the physician needs to talk to somebody that can kind of speak the medical jargon.
That can be helpful and just saying, Look, I do have somebody in healthcare who can have these conversations. But also just ensuring that you have an advocate with you, In the room. That you’re not going through this by yourself, to continue to say something’s wrong, to continue to let the physician know about it. Until something’s done.
MS: Well, I thank you for that. For all of the others who don’t have any idea about maternal mortality, thanks to Dr. Branch for what you’ve given us in understanding one advocate. Don’t go alone. Make sure you have one. Write your symptoms down. Keep a record during that moment to kind of give insight into when things are happening. Do not deny pain, share it loudly with the nurses and the physicians, so that you have it. But taking an advocate seems to be a real support so that everybody can pay attention, even if you are by yourself.
Find someone who can come and advocate or find out. Ask the hospital if you need an advocate at that moment. Make sure, but demand better care. I think that’s probably a message that I’d like to share. I want to thank you for health IQ, you’ve been phenomenal.