In the aftermath of global health crises, new research has shed light on the troubling neurological effects of severe infections. Groundbreaking studies reveal structural damage within one of the body’s most vital centers—the brainstem. This discovery could explain the lingering, life-altering symptoms experienced by many individuals long after the initial illness has passed.
Uncovering the neurological effects of infection
As the world moves beyond the immediate effects of recent health challenges, a significant portion of the population continues to struggle with persistent symptoms months or even years after recovering from severe infections. These post-infection complications, often described as long-term effects, are marked by overwhelming fatigue, cognitive difficulties, disrupted autonomic functions, and unexplained breathlessness that drastically reduce quality of life.
While past research has acknowledged broad neurological effects of severe infections, the specific mechanisms behind these lasting symptoms have remained unclear. Without clear answers, treatment has been inconsistent, leaving many individuals with few options for effective recovery.
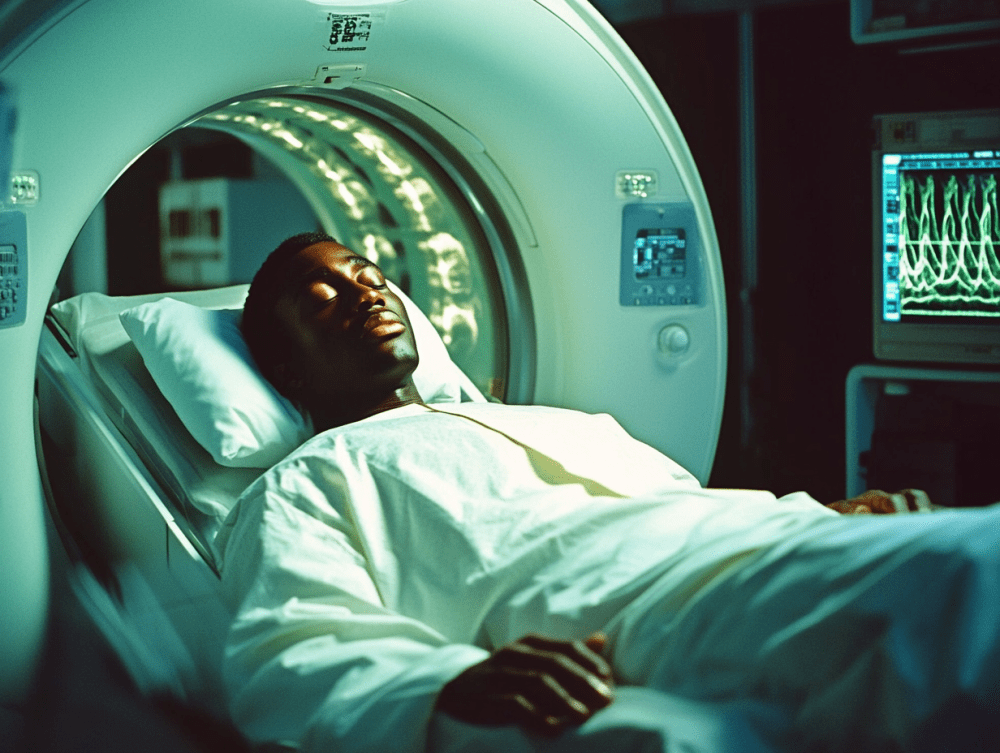
Recent advancements in imaging technology have made it possible to identify specific structural abnormalities within the brainstem—an essential region responsible for controlling fundamental survival functions such as breathing, heart rate, and consciousness.
Advanced imaging technology reveals structural damage
The research stands out due to its innovative use of ultra-high field magnetic resonance imaging. This technique, far more advanced than standard medical imaging, allows scientists to observe the brain in microscopic detail.
The study focused on individuals who had been hospitalized due to severe infections. Months after their treatment, researchers compared their brain scans with those of healthy individuals who had never experienced severe illness. The comparison revealed significant abnormalities in crucial areas of the brainstem, including regions responsible for respiratory control and autonomic function.
The medullary reticular formation—a network within the brainstem responsible for regulating breathing—showed notable structural changes. This could explain why some individuals experience persistent breathing difficulties long after their initial infection, even when their lung function appears normal.
The link between severity and brain changes
One of the most striking discoveries was the clear relationship between the severity of the initial illness and the extent of brain damage. Individuals who experienced the most severe symptoms showed more extensive structural changes within the brainstem.
This correlation suggests that brain damage may be directly related to how intense the infection was, not merely a random occurrence. The symptoms reported by those affected—such as ongoing breathlessness, fatigue, and cognitive fog—align with the areas of the brain found to be damaged.
This evidence points to a neurological explanation for symptoms that were previously misunderstood or dismissed. It suggests that, even after the infection clears, the lasting damage can continue to affect critical bodily functions.
The biological mechanisms driving brain damage
The research provides valuable insight into how severe infections cause brain damage without directly infecting brain cells. Rather than being a result of the virus itself invading the brain, the damage likely stems from the body’s immune response.
When the body fights off an infection, it releases inflammatory chemicals that can cross into the brain and trigger neuroinflammation. This process particularly affects the brainstem, which seems to be especially vulnerable.
Additionally, severe infections can impair blood flow to the brainstem, leading to localized oxygen deprivation. Since the brainstem requires a constant and rich oxygen supply to function properly, any disruption can result in significant damage.
Disrupted autonomic function and long-term symptoms
The brainstem plays a vital role in regulating automatic bodily functions—those that happen without conscious thought. When this part of the brain is damaged, it can result in a range of symptoms that seem unrelated but are deeply connected.
Disruptions to autonomic function may explain why individuals experience irregular heart rates, blood pressure issues, and digestive difficulties long after their initial infection. The affected areas also regulate alertness and wakefulness, offering a likely explanation for the profound fatigue that many report.
This research shows that post-infection symptoms often dismissed as psychological are rooted in measurable neurological damage. Understanding this connection could lead to better treatment strategies and provide validation for those experiencing these life-altering symptoms.
Implications for treatment and future research
These findings carry important implications for how long-term symptoms after severe infections are managed. By establishing a clear connection between infection severity and brainstem damage, researchers are shifting the focus from treating isolated symptoms to addressing underlying neurological damage.
This knowledge opens the door for targeted treatments that reduce neuroinflammation or promote neural repair. Therapies aimed at supporting brain health could potentially ease symptoms and improve quality of life for those suffering from long-term complications.
Early detection will also be crucial. Advanced brain imaging and thorough neurological assessments could help identify individuals at risk of developing long-term symptoms, allowing for earlier intervention and more effective treatment strategies.
Expanding our understanding of post-viral conditions
While this research focuses on severe infections, its implications extend far beyond one illness. Similar long-term symptoms have been documented after other viral infections, suggesting that brain damage from post-viral syndromes may be more common than previously thought.
As research continues, scientists are increasingly acknowledging that many post-infection symptoms previously categorized as psychological may, in fact, have clear biological origins. This evolving understanding could transform how post-viral syndromes are diagnosed, treated, and prevented.
A new era for neurological research
The discovery of structural brain damage following severe infections could mark a turning point in how post-infection health challenges are addressed. With this new understanding, future research can focus on preventing long-term neurological damage and developing more effective treatments for those already affected.
This groundbreaking work not only reshapes our understanding of brain health but also offers hope for millions worldwide seeking answers and solutions to persistent symptoms after severe infections.