That slight fever and headache your child woke up with? Most of the time, it’s nothing serious. But sometimes, those seemingly innocent symptoms can be the first whispers of something far more dangerous – meningitis, an infection that can go from mild concern to life-threatening emergency within hours.
Meningitis inflames the protective membranes surrounding the brain and spinal cord. While it’s relatively rare, it demands immediate attention when it strikes. The challenge for parents lies in distinguishing its early symptoms from common childhood illnesses, especially since young children can’t always articulate exactly what they’re feeling.
Understanding meningitis isn’t about living in fear but being equipped with knowledge that could make all the difference if your child ever faces this infection. Let’s explore what every parent should know about recognizing, preventing, and responding to childhood meningitis.
The deceptive early warning signs
Symptoms that mimic everyday illnesses
Meningitis often begins with symptoms easily mistaken for flu, common cold, or other routine childhood illnesses. Fever, headache, and tiredness – the typical suspects in many childhood ailments – frequently mark the initial phase of meningitis.
What makes early detection challenging is that children with meningitis might initially seem only mildly ill. They might continue playing or eating normally during the first few hours, creating a false sense of security. This deceptive mildness explains why parents sometimes delay seeking medical help until symptoms escalate dramatically.
The progression timeline matters enormously. With bacterial meningitis – the most dangerous form – a child can deteriorate from seemingly mild illness to critically ill within 12-24 hours. This rapid progression distinguishes meningitis from most common childhood infections, which typically develop more gradually.
The neck pain connection
As meningitis advances, neck stiffness or pain often develops. This isn’t the mild neck discomfort many of us experience after sleeping awkwardly – it’s more intense and has a specific cause. The inflammation of the meninges (the membranes around the brain and spinal cord) makes bending the neck forward particularly painful.
With young children, testing for this symptom can be challenging. One sign to watch for is resistance when you try to bend their head forward toward their chest during a diaper change or while dressing them. Older children might complain that they can’t touch their chin to their chest or that it hurts too much to try.
This neck stiffness doesn’t always appear immediately, which is why waiting for it before seeking medical help can be dangerous. Consider it a definitive sign rather than an early warning – if you notice this symptom, seek emergency medical care immediately.
The red flags that demand immediate action
The skin test everyone should know
One of the most distinctive signs of bacterial meningitis is a rash that doesn’t fade under pressure. This rash consists of small, red or purple spots that can appear anywhere on the body. Unlike most rashes, these spots don’t temporarily blanch (turn white) when pressed.
You can perform a simple test by pressing a clear glass firmly against the rash. If the spots remain visible through the glass rather than fading, this indicates a medical emergency requiring immediate hospital care. This “glass test” can help identify a meningococcal rash, associated with one of the most dangerous forms of bacterial meningitis.
Not all meningitis cases produce this rash, and sometimes it appears relatively late in the infection’s progression. Never wait for a rash to appear if other meningitis symptoms are present, but always take this sign seriously if you do notice it.
Light and noise sensitivity beyond normal
Children with meningitis often develop heightened sensitivity to light and sound as the infection progresses. This isn’t just finding bright light annoying – it’s genuine pain or significant distress when exposed to normal lighting or everyday noise levels.
You might notice your child keeping their eyes tightly shut in a normally lit room, covering their ears during regular conversation, or becoming unusually irritable when exposed to sensory stimulation they normally tolerate well. This sensitivity stems from inflammation of the brain tissue and surrounding membranes, making normal sensory input painful.
This symptom can be particularly telling in infants, who might cry inconsolably when picked up or exposed to normal household light and sound. In older children, complaints about room lights being “too bright” or normal speaking voices being “too loud” warrant attention, especially when combined with other symptoms.
The unusual body positions that signal trouble
Children with advancing meningitis sometimes adopt specific body positions due to the inflammation affecting their nervous system. The most concerning of these is opisthotonus – where the head and neck arch backward while the rest of the body remains stiff.
In infants, persistent arching of the back during an illness can signal meningitis. They might also show unusual rigidity when being held or resist being picked up due to pain and discomfort. These positions result from irritation of the meninges and increased pressure in the brain.
Another position-related warning sign appears during sleep. Children with meningitis often cannot or will not lie flat. They might insist on keeping their head elevated or seem unable to get comfortable in their normal sleeping position. This behavior stems from the increased pressure causing pain when they lie down.
Age-specific signals parents should know
The infant warning system
Babies can’t tell you about their headache or explain that light hurts their eyes, making meningitis particularly dangerous in infants. Instead, they communicate through behavioral changes that careful parents can learn to recognize.
A high-pitched, moaning cry unlike your baby’s normal crying deserves immediate medical attention. This distinctive cry, sometimes called “the meningitis cry,” signals significant neurological irritation. Similarly, excessive irritability where nothing comforts your normally consolable baby could indicate meningitis.
Changes in alertness represent another crucial warning sign. A previously alert baby who becomes difficult to wake or seems unusually drowsy needs prompt medical evaluation. At the other extreme, some infants with meningitis become hyper-alert with a wide-eyed, staring appearance and increased startle response to normal stimulation.
Feeding patterns often change dramatically with meningitis. A typically eager eater who suddenly refuses the breast or bottle, or seems unable to coordinate sucking and swallowing, might be showing signs of neurological involvement. Vomiting despite minimal feeding is particularly concerning.
Toddler and preschooler indicators
Children between ages 1-5 present their own set of challenges when it comes to identifying meningitis. Their developing communication skills might let them tell you “my head hurts” or “my neck hurts,” but they often lack the vocabulary to describe these sensations precisely.
Behavior changes often provide the earliest clues in this age group. A normally active toddler who suddenly wants to be held constantly or refuses to play deserves medical attention. Likewise, a child who seems confused, doesn’t recognize familiar objects or people, or shows significant personality changes needs immediate evaluation.
Pay particular attention to complaints about headache in this age group, especially when accompanied by vomiting. While many childhood illnesses cause headache, the headache of meningitis typically grows progressively worse and often focuses at the front of the head. When a young child clutches their head in obvious pain, take it seriously.
School-age children and teenagers
Older children can better articulate their symptoms, but other factors often complicate meningitis recognition in this age group. Pre-teens and teens might minimize complaints to avoid missing school events or activities, potentially delaying diagnosis.
The headache in older children with meningitis typically feels different from ordinary headaches. Kids might describe it as the “worst headache ever” or say it feels like their head is going to “explode.” This severe pain often localizes to the forehead and doesn’t respond well to over-the-counter pain relievers.
Confusion, difficulty concentrating, or unusual drowsiness in a normally alert older child warrants immediate medical attention. A teenager who comes home from school and goes straight to bed, skipping meals and activities they usually enjoy, might be showing early signs of a serious infection rather than typical teenage fatigue.
Prevention strategies every family should implement
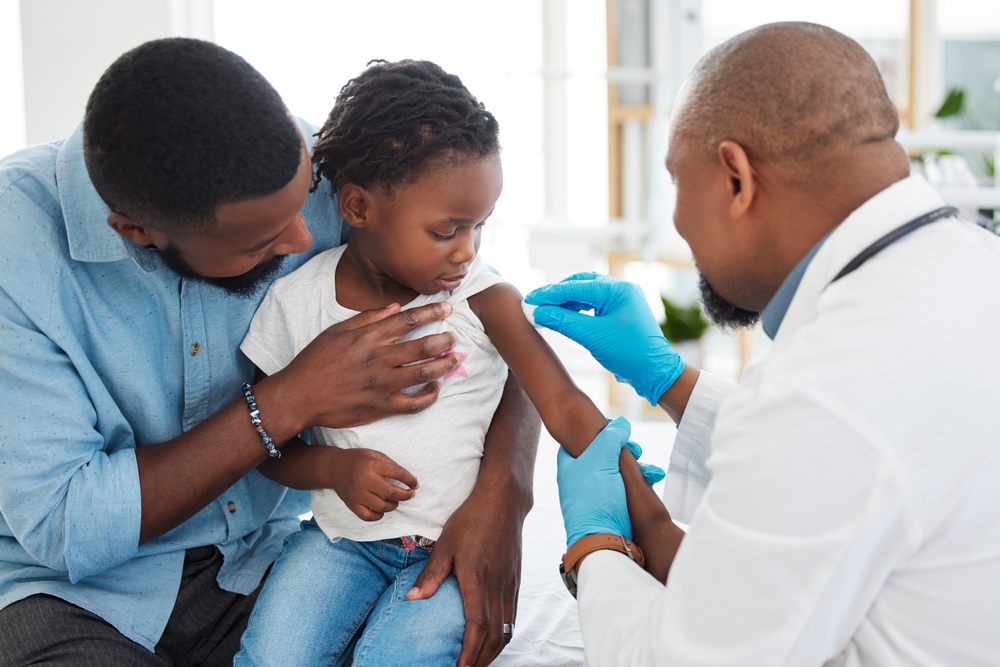
The vaccination conversation
Vaccines represent the most powerful protection against several types of bacterial meningitis. The childhood vaccination schedule includes immunizations against Haemophilus influenzae type b (Hib), pneumococcal bacteria, and meningococcal disease – all potential causes of bacterial meningitis.
The timing of these vaccines aligns with periods of highest vulnerability. The Hib and pneumococcal vaccines begin in infancy, while meningococcal vaccines typically start between ages 11-12 with a booster around age 16. This later vaccine timing targets adolescents, who face increased risk of meningococcal disease.
College-bound teenagers deserve special attention regarding meningitis protection. The close-living quarters of dormitories increase meningococcal disease risk, making the vaccine particularly important before campus move-in. Some colleges and universities now require proof of meningococcal vaccination before enrollment.
Everyday habits that reduce risk
Beyond vaccines, simple hygiene practices significantly reduce meningitis risk. Regular handwashing disrupts transmission of many infections that can lead to meningitis. Teaching children to wash thoroughly, especially before eating and after using the bathroom, provides protection against numerous illnesses.
Avoiding shared drinks, utensils, lip products, or toothbrushes prevents the exchange of saliva, which can transmit meningitis-causing organisms. This practice becomes particularly important for teenagers, who might be less careful about such sharing among friends.
Maintaining overall health through adequate sleep, good nutrition, and prompt treatment of ear and sinus infections helps prevent the conditions that sometimes precede meningitis. A strong immune system provides better defense against the pathogens that can invade the meninges.
When to get medical help and what to expect
The decision that can’t wait
With meningitis, the window for seeking medical care is measured in hours, not days. If you suspect meningitis based on a combination of symptoms, particularly fever plus headache plus any of the more specific signs we’ve discussed, seek emergency medical evaluation immediately.
The stakes of this decision are enormously high. Bacterial meningitis treated in its early stages typically responds well to antibiotics with excellent outcomes. The same infection left untreated for even 12-24 hours can lead to permanent neurological damage or death.
When in doubt, choose emergency care over waiting to see if symptoms improve. Explain your specific concerns about meningitis to medical staff upon arrival, as this can expedite the triage process and ensure appropriate testing. The worst outcome of seeking help is discovering it wasn’t meningitis – a huge relief compared to the alternative of waiting too long.
The diagnostic process
When meningitis is suspected, doctors typically perform a lumbar puncture (spinal tap) to analyze the cerebrospinal fluid surrounding the brain and spinal cord. While this procedure sounds frightening, it provides the most definitive diagnosis and guides proper treatment.
Blood tests, sometimes including blood cultures to identify bacterial infections, often accompany the lumbar puncture. Imaging studies like CT scans might precede the spinal tap if there’s concern about increased pressure in the brain that could make the procedure risky.
Doctors typically start antibiotics immediately if bacterial meningitis seems likely, even before test results confirm the diagnosis. This rapid treatment can be life-saving and reduces the risk of complications. The specific antibiotics might change once test results identify the exact organism causing the infection.
The bottom line
Meningitis deserves its reputation as a parent’s nightmare, but knowledge transforms fear into empowerment. Understanding the warning signs, knowing when to seek help, and maintaining prevention measures dramatically reduces the threat this infection poses to your child.
The most important takeaway? Trust your instincts and act quickly when symptoms concern you. The subtle difference between meningitis and common childhood illnesses often lies in the rapid progression and the combination of symptoms rather than any single sign.
Remember that most children with fever and headache don’t have meningitis, but those who do need medical intervention without delay. In the arena of serious childhood infections, it’s always better to seek unnecessary medical care than to miss or delay necessary treatment. Your vigilance and prompt action could make all the difference if your child ever faces this challenging infection.