The human body can survive weeks without food, but only days without water. Yet millions of people walk around in a state of chronic dehydration, completely unaware that their kidneys are slowly deteriorating with each passing day. These remarkable organs, no larger than computer mice, filter approximately 50 gallons of blood daily while maintaining the delicate chemical balance that keeps every cell in the body functioning properly.
When water intake falls short of the body’s needs, the kidneys face an impossible task. They must continue their essential work of filtering waste, regulating blood pressure, and maintaining fluid balance while operating with insufficient resources. This creates a cascade of problems that can permanently damage these irreplaceable organs and set the stage for life-threatening complications.
The relationship between hydration and kidney function extends far beyond simple thirst. Dehydration triggers a complex series of physiological changes that force the kidneys to work harder, operate less efficiently, and eventually begin to fail. Understanding these mechanisms reveals why proper hydration represents one of the most critical yet overlooked aspects of preventive healthcare.
Most people dramatically underestimate their daily water needs and overestimate their actual intake. The consequences of this miscalculation compound over time, creating kidney damage that often goes undetected until it reaches advanced stages. By the time symptoms appear, significant and potentially irreversible harm has already occurred.
Blood concentration reaches dangerous levels
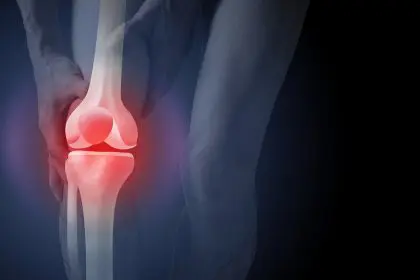
When the body lacks adequate water, the blood becomes increasingly concentrated with waste products, minerals, and other substances that should be diluted and efficiently processed. This thickened blood places enormous strain on the kidneys as they struggle to filter higher concentrations of toxins through their delicate filtration units called nephrons.
The kidneys contain approximately one million nephrons each, and these microscopic structures cannot regenerate once damaged. As blood concentration increases due to dehydration, these nephrons must work exponentially harder to maintain normal filtration rates. The increased workload causes inflammation and scarring that permanently reduces kidney function.
Concentrated blood also moves more slowly through the kidney’s intricate network of tiny blood vessels. This sluggish circulation reduces the efficiency of waste removal and creates areas of stagnation where harmful substances can accumulate. Over time, these deposits can form crystals and stones that cause excruciating pain and further damage to kidney tissue.
The minerals and waste products in concentrated blood can reach levels that exceed the kidneys’ ability to process them safely. Calcium, uric acid, and other substances begin to precipitate out of solution, forming deposits that clog the kidneys’ filtration system and create permanent obstructions that reduce overall function.
Blood pressure also rises as the cardiovascular system works harder to pump thickened blood through the body’s circulatory network. This elevated pressure damages the delicate blood vessels within the kidneys, creating scarring that further impairs their ability to filter waste effectively.
Waste removal efficiency plummets dramatically
Dehydration severely compromises the kidneys’ primary function of removing metabolic waste from the bloodstream. Under normal circumstances, adequate water flow helps flush toxins through the kidneys and out of the body efficiently. When water becomes scarce, this flushing action slows to a crawl, allowing dangerous substances to accumulate.
The kidneys produce urine by filtering water and waste from the blood, then reabsorbing essential nutrients and the right amount of water back into circulation. Dehydration disrupts this precise process by forcing the kidneys to reabsorb more water than optimal, concentrating waste products to dangerous levels in the remaining urine.
Highly concentrated urine creates a toxic environment within the kidneys that damages the delicate cells lining the urinary tract. This damage increases the risk of infections, stone formation, and chronic inflammation that can progress to permanent kidney disease over time.
The buildup of waste products in the blood due to poor kidney filtration affects every organ system in the body. Brain function, heart rhythm, muscle contraction, and cellular metabolism all depend on the kidneys maintaining proper chemical balance. When dehydration impairs this function, the entire body suffers.
Certain waste products become particularly problematic when concentrated due to dehydration. Urea, creatinine, and other nitrogen-containing compounds can reach toxic levels that poison cells throughout the body. The kidneys themselves become primary victims of this toxicity, creating a vicious cycle of declining function.
Electrolyte balance becomes dangerously unstable
The kidneys serve as the body’s master chemists, precisely regulating the levels of sodium, potassium, calcium, phosphorus, and other essential minerals in the blood. Dehydration throws this delicate balancing act into chaos, creating electrolyte imbalances that can trigger heart rhythm abnormalities, muscle weakness, and neurological dysfunction.
When water levels drop, the kidneys retain more sodium to help the body hold onto whatever fluid remains available. This sodium retention leads to fluid accumulation in tissues, causing swelling in the legs, ankles, and around the eyes. The excess sodium also contributes to high blood pressure that further damages kidney blood vessels.
Potassium regulation becomes particularly problematic during dehydration. The kidneys may either retain too much potassium, leading to dangerous heart rhythm disturbances, or lose excessive amounts, causing muscle weakness and cramping. Both scenarios can have life-threatening consequences if left uncorrected.
Calcium and phosphorus balance also becomes disrupted when dehydration impairs kidney function. These minerals play crucial roles in bone health, muscle function, and cellular processes throughout the body. Imbalances can lead to bone weakening, muscle spasms, and metabolic dysfunction that affects energy production in every cell.
The acid-base balance of the blood, another critical kidney function, becomes increasingly unstable as dehydration progresses. The kidneys must maintain blood pH within a very narrow range for proper cellular function. Dehydration makes this regulation more difficult, potentially leading to acidosis or alkalosis that can be fatal if severe.
Kidney stone formation accelerates rapidly
Dehydration creates ideal conditions for kidney stone development by concentrating minerals and reducing the fluid available to keep them dissolved in solution. These painful deposits form when substances like calcium, oxalate, and uric acid reach concentrations that exceed the urine’s ability to keep them dissolved.
The most common kidney stones contain calcium oxalate, which crystallizes more readily in concentrated urine. Dehydration reduces urine volume and increases the concentration of both calcium and oxalate, dramatically increasing the likelihood of stone formation. Once stones begin forming, they can grow rapidly in the concentrated environment.
Uric acid stones represent another serious consequence of dehydration. These stones form more easily in acidic urine, and dehydration tends to make urine more acidic while concentrating uric acid levels. People who consume high-protein diets face particularly high risks when dehydrated, as protein metabolism produces large amounts of uric acid.
The physical trauma of passing kidney stones can cause additional damage to the kidneys and urinary tract. Sharp crystal edges scrape and tear delicate tissues, creating bleeding, scarring, and increased susceptibility to infections. Large stones may completely block urine flow, creating emergency situations that require immediate medical intervention.
Recurrent kidney stones often indicate chronic dehydration and ongoing kidney damage. Each stone episode causes inflammation and scarring that reduces overall kidney function. People who experience multiple stone episodes without addressing underlying dehydration face progressive kidney deterioration over time.
Blood pressure regulation fails completely
The kidneys play a central role in blood pressure regulation through multiple mechanisms that become severely compromised during dehydration. These organs control fluid volume, produce hormones that affect blood vessel constriction, and filter substances that influence cardiovascular function throughout the body.
When dehydration reduces blood volume, the kidneys respond by activating the renin-angiotensin-aldosterone system, a complex hormonal cascade designed to raise blood pressure and retain fluid. While this response may be appropriate for short-term dehydration, chronic activation leads to persistently elevated blood pressure that damages blood vessels throughout the body.
The kidneys also produce hormones that directly affect blood vessel tone and heart function. Dehydration disrupts the production and balance of these hormones, leading to unpredictable blood pressure fluctuations that strain the cardiovascular system and reduce the efficiency of blood flow to vital organs.
High blood pressure caused by dehydration creates a destructive cycle within the kidneys themselves. Elevated pressure damages the tiny blood vessels that perform filtration, reducing kidney function and making blood pressure regulation even more difficult. This progressive deterioration can eventually lead to complete kidney failure.
The relationship between dehydration, kidney function, and blood pressure becomes particularly dangerous in people who already have cardiovascular risk factors. Existing heart disease, diabetes, or other conditions can accelerate the kidney damage caused by chronic dehydration, leading to rapid progression toward kidney failure.
Infection resistance drops to dangerous lows
Proper hydration plays a crucial role in preventing urinary tract infections and other kidney-related infections. Adequate water intake helps flush bacteria and other pathogens from the urinary system before they can establish infections that can spread to the kidneys themselves.
Dehydration reduces urine production and creates stagnant conditions within the urinary tract that favor bacterial growth. Concentrated urine also provides a nutrient-rich environment where harmful bacteria can multiply rapidly, increasing the risk of bladder infections that can ascend to the kidneys.
The immune system’s ability to fight infections becomes compromised when dehydration affects kidney function. The kidneys help maintain proper immune cell function through their role in producing certain hormones and maintaining chemical balance. When kidney function declines, the body’s infection-fighting capabilities diminish accordingly.
Kidney infections represent serious medical emergencies that can lead to permanent kidney damage, sepsis, and death if not treated promptly. People with chronic dehydration face higher risks of developing these dangerous infections and may experience more severe complications when infections do occur.
The scarring and inflammation caused by recurrent urinary tract infections further reduce kidney function, creating a downward spiral of declining health. Each infection episode damages delicate kidney tissues, making future infections more likely and more severe.
Toxin accumulation reaches critical thresholds
The kidneys serve as the body’s primary detoxification system, filtering environmental toxins, medication byproducts, and metabolic waste from the bloodstream. Dehydration severely compromises this essential function, allowing dangerous substances to accumulate to levels that can cause organ damage throughout the body.
Many common medications depend on adequate kidney function for safe elimination from the body. When dehydration impairs kidney function, these medications can accumulate to toxic levels that cause serious side effects or organ damage. This becomes particularly dangerous for people taking multiple medications or those with existing health conditions.
Environmental toxins from air pollution, chemicals in food and water, and occupational exposures normally get filtered out by healthy kidneys. Dehydration reduces this protective function, allowing toxins to circulate longer and reach higher concentrations in body tissues. The kidneys themselves become primary targets for this accumulated toxicity.
The liver works closely with the kidneys to process and eliminate toxins from the body. When kidney function declines due to dehydration, the liver must work harder to compensate, potentially leading to liver damage and further impairment of the body’s detoxification capabilities.
Chronic toxin accumulation affects brain function, hormone production, immune system activity, and cellular energy production throughout the body. The gradual poisoning that results from impaired kidney function due to dehydration can cause fatigue, cognitive dysfunction, and increased susceptibility to various diseases.
Recovery becomes increasingly difficult
Once dehydration has caused significant kidney damage, recovery becomes a slow and often incomplete process. Unlike some organs that can regenerate damaged tissue, the kidneys have limited ability to repair themselves once nephrons are destroyed or severely scarred.
The progression from acute dehydration to chronic kidney disease often goes unnoticed until damage becomes severe. Early stages of kidney dysfunction produce few symptoms, allowing the deterioration to continue unchecked for years. By the time people notice changes in urination, energy levels, or other symptoms, substantial damage has already occurred.
Reversing dehydration-related kidney damage requires not only adequate fluid intake but also comprehensive medical management to address complications like high blood pressure, electrolyte imbalances, and accumulated toxins. This process can take months or years and may never restore full kidney function.
People with chronic kidney disease face numerous lifestyle restrictions and require ongoing medical monitoring to prevent further deterioration. Dietary changes, medication adjustments, and regular laboratory testing become necessary to manage the condition and prevent progression to complete kidney failure.
The financial and emotional costs of kidney disease treatment can be overwhelming. Dialysis, kidney transplantation, and ongoing medical care represent enormous expenses that could often be prevented through proper hydration and early intervention.
Understanding the devastating effects of dehydration on kidney function empowers people to take proactive steps to protect these vital organs. The simple act of maintaining adequate hydration can prevent enormous suffering and preserve kidney health for a lifetime. The choice between drinking enough water and facing potential kidney failure represents one of the most important health decisions people make every day, often without realizing the profound consequences of their choice.