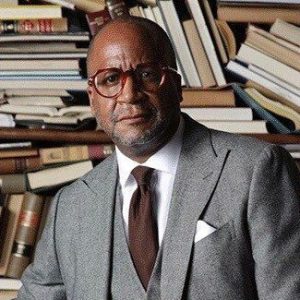
In a compelling Health IQ interview, Dr. Kanzoni Asabigi, Vice President of Detroit Recovery Project, brings his extensive public health expertise to address the critical intersection of HIV and addiction. With more than three decades of health care leadership experience and a distinguished academic background, Dr. Asabigi shares vital insights on this often-overlooked connection, drawing from his work at the premier recovery organization providing services to individuals battling substance use disorders.
How do HIV and addiction intersect in our communities?
This is a really very important topic, I am vice president here at Detroit Recovery Project, we are the premier recovery organization, providing services to individuals in recovery, and individuals that are suffering from substance use disorders, and seek to be in recovery.
HIV is a very, very important topic, but we don’t talk more about it, because most often it involves sex, and sometimes some people just shy away from talking about sex.
And the link with addiction is that, you know, when people are suffering from this disease, they don’t think clearly. Most often, if they are actively in addiction, so sometimes the choices they make, who they are with, they may not be taking the necessary precautions, using a condom, for example, engaging in sex.
The other piece also is that we have individuals sometimes inject drugs, if they inject drugs and share needles, they are at risk of contracting HIV through that, but we’ve come a long, long way from the days when the diagnosis was a death sentence, when people got diagnosed with HIV back in the eighties. Now, people can live a normal life, if they are in treatment.
How does your organization approach the HIV-addiction connection?
What we do here at Detroit Recovery Project is that we provide treatment for individuals suffering from substance use disorders and mental health, but we also engage in what we call harm reduction.
So what it means is that we meet people where they are, if they are still using, we give them clean needles to use and not to share, and this is public health 101. We’ve seen that it has reduced the HIV transmission amongst individuals using drugs by injection.
How does the issue of sex work and addiction impact HIV transmission?
That’s something that you know we do here at Detroit Recovery Project with harm reduction, one, we try to engage people in those situations suffering from substance use disorders to get into treatment.
If we don’t. If they are not ready, we have an abundant supply of condoms, and we say, if you’re going to engage in any sexual activity, use a condom either yourself or the person that is, you know, you’re going to have the sex with. And then the other thing is that with HIV we provide counseling and testing right then, but the key is to engage people to get them into treatment, and we know that engaging people being in touch with them all the time, making sure that they know that you know somebody’s there for them when they want to get into treatment.
We just encourage protected sex, whatever the form, making sure that there’s no exchange of bodily fluids. Usually, either vaginally or anal and make sure that they do not share needles to reduce the risk of HIV transmission.
In addition to that, we also see that people, in those situations contract other STIs, we’ve seen a rise in syphilis cases, we’ve seen a rise in gonorrhea, but we want to make sure that people get treated and have protected sex, but, more importantly, encourage them to get into treatment.
What specific concerns exist for Black women regarding HIV infection rates?
That’s a really serious issue amongst the Black population, and we’ve seen a disproportionate HIV infection amongst heterosexuals, and as you mentioned Black women, especially older Black women, they engage in sexual activity, and that’s normal, but it’s important to make sure that, one, they know their own status.
And two, to be open with a partner asking the right questions about their status when it comes to HIV. It’s very important that they use protection at all times, until they are comfortable that they are in a monogamous relationship and trust each other, that the other person is not going to have sexual activity outside of the relationship they have together, if they’re together for a long time.
What’s the current state of HIV treatment and stigma?
It’s always very, very important to know one’s status, once that is known, you can then be comfortable, if it’s negative, to take the necessary precautions that are necessary to engage in any sexual activity.
If the test comes back positive, then it’s very important that some other action be taken, that means getting to the doctor, get into treatment as soon as possible.
We have ART, Antiretroviral therapy, people shouldn’t die prematurely from just contracting HIV, now the expectation is that people can live a normal life throughout their lifespan, but if they are not in treatment, then that becomes problematic and they can get complications by not being in treatment. So it’s very important for individuals that are HIV-positive to be in treatment so that the doctor can monitor the viral load to the point that is not detectable.
Once it’s not detectable, we now also know that it’s not transmissible. So U equals U, undetectable and untransmittable, but, we see a lot of new cases in the South, the southern part of the country according to CDC. So, we need your geographic location is very important for the Black community to be aware of.
How important is regular testing and communication with health care providers?
Sometimes, it’s good to have questions prepared when you go to see your doctor so that you don’t forget what the questions you want to ask. It’s important to get an annual physical and then ask the doctor, in addition to everything, they talk about diabetes, they talk about high blood pressure, asthma, talk about your sexual health.
Be open about it, it’s you and your doctor, what you talk with your doctor is confidential. Ask any questions about HIV and other STIs, especially if you are sexually active and have more than one partner.
Not all the information that comes through the iPhone and text, and what they call X and WhatsApp and all that, is accurate, but a health care provider will have the right information and give it to you in the way that you can understand, but you have to ask the question.