The United States has made remarkable progress in fighting air pollution since implementing the Clean Air Act in 1970, with emissions of major pollutants dropping by 78% over five decades. Yet this victory masks a troubling reality: millions of Americans, particularly those with asthma in communities of color, continue breathing unhealthy air both outdoors and inside their homes, leading to increased respiratory emergencies and chronic health complications. Current data shows that poor air quality triggers asthma attacks in vulnerable populations at an alarming rate, with children and elderly residents facing the highest risks.
A matter of life and death
Air pollution emerges as the most significant external threat to human longevity, cutting global life expectancy by approximately 2.3 years. This reduction surpasses the impact of widely recognized health threats like alcohol use and transportation accidents. For the 25 million Americans living with asthma, poor air quality can trigger severe attacks, force emergency hospital visits, and create chronic health complications.
Urban air crisis
The stark divide between urban and rural air quality reveals a troubling pattern. City residents, representing about 80% of the U.S. population, face extremely poor air quality for nearly 48 days each year. In contrast, rural communities experience just four such days annually. This disparity becomes even more significant when examining its impact on vulnerable populations, particularly children and elderly residents in urban areas.
The racial divide in air quality
Recent studies uncover disturbing patterns in how air pollution affects different racial groups. Black and Hispanic communities consistently face higher exposure to harmful air pollutants than predominantly white neighborhoods. This disparity stems from decades of discriminatory practices, including historical redlining policies that forced communities of color into areas with greater industrial activity and higher pollution levels.
Asthma’s unequal burden
The health implications of these environmental inequities appear starkly in asthma statistics. Black Americans face a 42% higher likelihood of developing asthma compared to their white counterparts. Puerto Rican communities report the highest asthma rates among all ethnic groups in America. Perhaps most alarming, American Indian and Alaskan Native children show 50% higher asthma rates than other groups.
The legacy of discrimination
Historical housing discrimination continues to shape modern health outcomes. Communities historically subjected to redlining typically experience higher pollution levels, worse environmental conditions, and limited access to healthcare resources. These areas often cluster near industrial zones, major highways, and other sources of air pollution, creating a cycle of environmental and health challenges.
Healthcare access barriers
The impact of air quality disparities extends beyond immediate health effects. Many residents in affected communities rely heavily on emergency rooms for asthma treatment rather than maintaining relationships with primary care providers. This pattern of crisis-driven healthcare often results in worse outcomes and higher medical costs for families already facing economic challenges.
Inside the home
Indoor air quality presents another critical challenge, particularly in low-income housing. Aging infrastructure, poor ventilation systems, and the presence of gas stoves contribute to indoor air pollution. Recent initiatives, like The Children’s Hospital of Philadelphia’s CAPP+ Home Repairs Program, demonstrate how addressing these indoor environmental factors can significantly improve asthma outcomes.
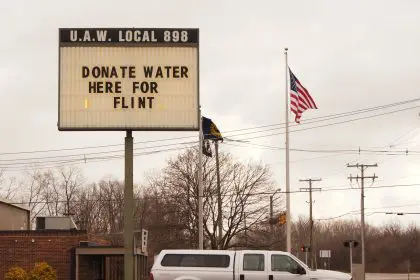
Community solutions emerge
Grassroots efforts to combat these disparities show promising results. Local organizations partner with healthcare providers to create asthma management programs tailored to specific community needs. These initiatives often combine medical care with environmental improvements, addressing both immediate health concerns and underlying environmental factors.
Policy changes needed
Addressing air quality disparities requires comprehensive policy reform. Environmental justice advocates push for stricter regulations on industrial emissions in urban areas, improved monitoring of air quality in vulnerable communities, and increased funding for clean air initiatives. These efforts aim to create more equitable environmental conditions across all neighborhoods.
The role of climate change
Climate change amplifies existing air quality challenges. Rising temperatures increase the formation of ground-level ozone, while longer wildfire seasons contribute to particulate pollution. These changes disproportionately affect communities already struggling with poor air quality, creating new urgency for environmental justice initiatives.
Moving toward solutions
Progress in addressing these disparities requires a multi-faceted approach. Healthcare providers increasingly recognize the need for culturally competent asthma care that considers environmental and social factors. Community organizations work to improve access to preventive care and environmental modifications that can reduce asthma triggers in homes.
The path forward
The connection between air quality and asthma underscores the urgent need for environmental justice. As communities continue fighting for cleaner air and better health outcomes, success requires addressing both immediate health needs and the systemic inequities that create and perpetuate these disparities. The right to breathe clean air remains fundamental to public health and social justice.