Asthma affects approximately 25 million Americans, including 5.1 million children, according to the Asthma and Allergy Foundation of America. While many experience mild symptoms that respond well to medication, severe asthma attacks remain a frightening and potentially life-threatening emergency that demands immediate action.
Knowing how to respond when someone struggles to breathe can mean the difference between life and death. Whether you’re a parent, teacher, coworker, or friend, understanding the proper steps to take during a severe asthma attack equips you with crucial skills for emergency situations.
How to recognize a severe asthma attack
Before taking action, it’s important to differentiate between typical asthma symptoms and a severe attack requiring emergency intervention. During a severe asthma attack, a person may display several alarming signs:
Severe breathing difficulty – The person struggles to breathe even while sitting still or lying down. Their chest may visibly heave with each breath attempt.
Blue-tinged lips or fingernails – This discoloration, called cyanosis, indicates insufficient oxygen in the blood and represents a medical emergency.
Inability to speak full sentences – The person can only say a few words before needing to catch their breath.
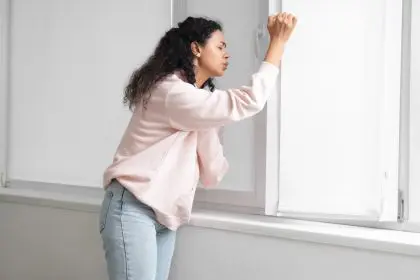
Hunched shoulders and forward-leaning posture – This position indicates the person is using accessory muscles to help breathe.
Retraction between ribs or at the neck – The skin between ribs or at the base of the throat pulls inward during breathing attempts.
Confusion or altered mental state – Oxygen deprivation may cause disorientation or drowsiness.
No improvement after using rescue inhaler – Symptoms persist or worsen despite medication use.
These warning signs require immediate action, as delayed response during severe asthma attacks can lead to respiratory failure or even death in extreme cases.
The crucial first 7 steps to help during an asthma emergency
When someone experiences a severe asthma attack, follow these seven essential steps to provide potentially life-saving assistance:
- Stay calm and help the person sit upright – Panic worsens breathing difficulties. Guide the person to sit upright, ideally leaning slightly forward with arms supported on a table or knees. This position maximizes lung expansion and airflow. Never force someone having an asthma attack to lie down, as this compromises breathing further.
- Help administer quick-relief medication – Assist the person in using their rescue inhaler if they have one available. Most emergency inhalers contain albuterol, which rapidly relaxes airway muscles. Follow the person’s asthma action plan if known, typically two puffs with 30-60 seconds between each. Ensure proper inhaler technique for maximum effectiveness.
- Remove potential triggers – Quickly assess the environment for possible asthma triggers. Move away from smoke, strong fragrances, cold air, or other known irritants. If outdoors during high pollen or pollution days, move inside to filtered air if possible. For indoor attacks, consider moving outside if indoor allergens might be responsible.
- Encourage slow, controlled breathing – Coach the person to focus on exhaling completely before inhaling again, which helps prevent air trapping in the lungs. The pursed-lip breathing technique—inhaling slowly through the nose and exhaling through pursed lips—can help reestablish breathing control during an attack.
- Call emergency services immediately if the person’s symptoms don’t improve within 5-10 minutes of using rescue medication, the person doesn’t have their rescue inhaler available, the person shows signs of severe distress like blue lips or extreme difficulty breathing, the person becomes confused or loses consciousness and you have any doubt about the severity of the situation
- Continue monitoring until help arrives – Stay with the person continuously. Monitor their breathing pattern, coloration, and level of consciousness. If they have a peak flow meter, measurements below 50% of their personal best indicate severe attack. Be prepared to provide this information to emergency responders.
- Document the attack details – Once the emergency has passed, make notes about the timing, severity, potential triggers, and effectiveness of medications. This information helps healthcare providers adjust treatment plans and may reveal patterns to prevent future attacks.
What not to do during a severe asthma attack
Understanding what to avoid is equally important when helping someone during a respiratory emergency:
Don’t leave the person alone – Severe asthma attacks can escalate quickly. Continuous supervision ensures help if the situation worsens.
Don’t give the person someone else’s medication – Asthma medications aren’t interchangeable. Using another person’s prescription could cause adverse reactions or inadequate treatment.
Don’t offer food or drinks – Swallowing may become difficult during severe breathing distress, creating choking hazards.
Don’t place pillows behind the back – This encourages slumping, which restricts lung capacity. Instead, support upright posture.
Don’t delay calling emergency services when symptoms appear severe – The “wait and see” approach can have catastrophic consequences during respiratory emergencies.
Don’t transport the person yourself unless absolutely necessary – Emergency medical responders provide oxygen and advanced treatment en route to hospitals.
How emergency responders handle severe asthma attacks
When emergency services arrive, they implement specialized protocols for severe asthma attacks:
Medical professionals typically administer nebulized bronchodilators that deliver medication directly to the airways as fine mist, more effective than handheld inhalers during severe episodes. They may provide supplemental oxygen to increase blood oxygen levels and reduce strain on the respiratory system.
In hospital settings, medical teams may administer intravenous corticosteroids to rapidly reduce airway inflammation, conduct comprehensive lung function testing to assess severity, and monitor oxygen saturation levels continuously through pulse oximetry.
For extremely severe cases not responding to standard treatments, healthcare providers may consider advanced interventions like breathing support through BiPAP (Bilevel Positive Airway Pressure) or, rarely, intubation with mechanical ventilation for respiratory failure.
Creating an asthma action plan for future emergencies
After experiencing a severe asthma attack, working with healthcare providers to develop or update an asthma action plan becomes essential. These personalized plans typically include: Medication instructions for different severity levels; Peak flow meter readings with corresponding actions; Trigger identification and avoidance strategies; Clear guidelines for when to seek emergency care and; Emergency contact information for healthcare providers
Sharing this plan with family, friends, coworkers, and school personnel ensures everyone knows how to respond appropriately during future asthma emergencies.
When to consider additional medical intervention
Following a severe asthma attack, healthcare providers might recommend treatment adjustments or specialist referrals. Persistent symptoms despite current medication regimens may indicate the need for inhaled corticosteroid dosage adjustments, addition of long-acting bronchodilators, evaluation for biologic therapy for specific severe asthma types, assessment for underlying conditions worsening asthma control and pulmonologist referral for specialized management
Regular follow-up appointments help maintain optimal asthma control and prevent future severe episodes through proactive management strategies.
Preventing future severe asthma attacks
While knowing emergency response techniques remains vital, preventing severe attacks ultimately offers the best protection. Prevention strategies include:
Maintaining consistent use of controller medications even when feeling well prevents the underlying inflammation driving asthma exacerbations. Identifying and avoiding personal triggers through environmental modifications and lifestyle adjustments reduces attack frequency significantly.
Regular medical check-ups allow for treatment plan refinements before minor symptoms escalate to emergencies. For patients with frequent severe episodes, allergen immunotherapy or newer biologic treatments might provide additional protection beyond standard medications.
With proper education, preparation, and swift action, most asthma emergencies can be managed effectively. Understanding both how to prevent attacks and how to respond when they occur creates a comprehensive approach to asthma management that saves lives and improves quality of life for those with this chronic respiratory condition.