The morning alarm that signaled the need for an evacuation from the advancing Palisades fire sparked a profound shift in the lives of Los Angeles residents, but perhaps none were more acutely affected than mental health professionals. Their work had always been demanding, but the immediate transition to remote therapy and managing personal evacuation procedures in the midst of a natural disaster posed unforeseen challenges. This unprecedented situation forced a recalibration of priorities, testing the resilience of these professionals as they navigated both their personal safety and the needs of their patients.
Professional duties amid personal crisis
For mental health professionals, maintaining continuity of care during an evacuation was crucial. As the fire spread, many had to quickly pivot from in-person therapy sessions to virtual consultations, using online platforms to continue providing care. This transition required careful coordination, balancing the technical challenges of virtual platforms with the emotional demands of both the therapists and their patients. While some were frantically organizing essential documents and medications for their own families, they still had to remain focused and professional, offering the kind of support their patients depended on.
This shift to virtual services revealed not only the resilience of mental health professionals but also the importance of maintaining a consistent therapeutic relationship, even in the face of an active disaster. The unique nature of these circumstances demonstrated that mental health care isn’t simply about treating patients in a controlled environment, it’s also about adapting to unpredictable crises while delivering uninterrupted support.
Managing collective trauma
The collective trauma experienced by the community following the wildfire evacuation was felt far and wide, triggering an influx of mental health needs. The immediate concerns about property loss and safety were amplified by fears of the future, creating a volatile emotional environment. Mental health professionals found themselves at the heart of this crisis, trying to mitigate acute anxiety while also addressing the long-term psychological effects. Many individuals, struggling to cope with the uncertainty and devastation, turned to therapy sessions to find stability and comfort.
At the same time, therapists were contending with their own feelings of uncertainty and distress. The emotional toll of witnessing clients experience acute trauma while coping with the impact of the fire personally added an additional layer of complexity. This dual responsibility—caring for others while experiencing the same fears—demanded a balance of compassion and professionalism.
The intersection of personal and professional boundaries
One of the more complicated aspects of providing therapy during a crisis is navigating the intersection between personal experience and professional boundaries. Mental health professionals are trained to offer empathy, but in times of collective trauma, it’s difficult to separate personal emotions from the therapeutic process. In this case, the shared experience of evacuation brought therapists and patients closer, creating a dynamic in which personal stories of fear and loss were exchanged. While some patients found comfort in these shared experiences, therapists had to maintain a careful line between empathy and professionalism.
Mental health professionals worked hard to remain focused on patient needs, but the process was not without challenges. For many therapists, the act of acknowledging their own distress while caring for others required a new level of vulnerability and trust in their professional relationships. This blurring of personal and professional lines in therapy raised questions about the long-term impact on therapist well-being, as it added emotional weight to their already demanding roles.
Implementing crisis response strategies
As the fire raged on, mental health professionals developed and implemented several strategies to cope with both personal and professional challenges. For many, the first step was clear communication—both with their patients and among colleagues. Establishing accessible channels for communication ensured that patients could continue receiving the support they needed while therapists could stay informed about safety measures and evacuation updates.
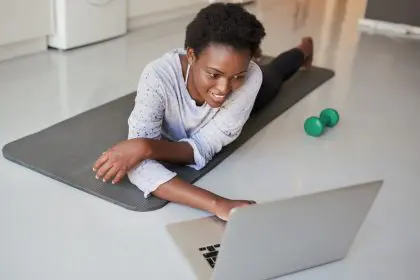
Additionally, therapists leaned into the use of flexible therapy delivery systems, which included telehealth platforms and secure online chat options. These platforms allowed therapists to provide continuous care even as they dealt with their own safety and security concerns. It was also essential to develop strong support networks among colleagues, as peer support provided emotional relief and practical advice during stressful moments. Regular self-care routines, which might include exercise or meditation, were critical in helping therapists maintain their own mental health while serving their patients.
Building community resilience
The wildfire crisis also highlighted the importance of community resilience. Mental health professionals across Los Angeles collaborated to provide support in innovative ways. Free group sessions and virtual support networks were developed, offering individuals affected by the fires a space to process their experiences collectively. These initiatives were designed not only to address immediate trauma but also to create lasting systems of support in the aftermath of the disaster.
The community-based response demonstrated the power of collective healing. By leveraging both traditional therapy approaches and virtual platforms, mental health professionals were able to extend their services to a broader population. This collective response fostered a sense of solidarity, helping the community cope with the aftermath of the fires and build resilience for the future.
Long-term implications for mental health care
The experience of providing mental health care during the Palisades fire evacuation has profound implications for the future of crisis response in the mental health community. This experience underlined the need for more robust emergency response protocols and flexible treatment modalities that can be adapted in times of crisis. The integration of virtual platforms into mental health care practices will likely continue to play a key role in ensuring continuity of care during emergencies. The lessons learned from this experience will undoubtedly shape future approaches to crisis management and patient care, helping mental health professionals remain prepared for the challenges posed by natural disasters.
As communities continue to face increasing instances of natural disasters, the mental health community’s ability to adapt and maintain care in the face of crises is critical. The experience of managing therapy during such a challenging time speaks to the resilience of both the professionals and the communities they serve. In the future, it will be essential for mental health professionals to continue developing crisis-response strategies and ensuring that the necessary infrastructure is in place to support both providers and patients.