Discovering a rash around your child’s mouth can trigger immediate concern for many parents. Though these unsettling red patches are frequently attributed to food allergies, the reality is much more nuanced. Understanding the various potential causes empowers parents to respond appropriately, whether that means simple home care or seeking urgent medical attention.
Common irritants that mimic allergic reactions
The area surrounding a child’s mouth is particularly vulnerable to irritation due to its frequent exposure to foods, saliva, and environmental elements. Many substances that aren’t true allergens can nonetheless trigger inflammatory responses that look remarkably similar to allergic reactions.
Acidic foods represent one of the most common culprits behind mouth rashes in children. Citrus fruits like oranges, lemons, and grapefruits contain natural acids that can irritate sensitive skin. Similarly, tomatoes and tomato-based products like pasta sauce or ketchup frequently cause temporary redness and irritation around the mouth.
These reactions typically appear immediately after consumption and resolve within hours without intervention. The distinctive pattern often forms around the lips in the exact areas where the food made contact with the skin. Unlike true allergic responses, these irritant reactions don’t typically involve the immune system and won’t cause systemic symptoms.
Parents can differentiate these irritant reactions from allergies by noting whether symptoms appear only where the food touched the skin and whether they resolve quickly without treatment. Applying a thin layer of petroleum jelly around the mouth before serving acidic foods can create a protective barrier that prevents these reactions.
Infectious causes requiring different approaches
Viral and bacterial infections frequently manifest with mouth-area rashes that parents might initially mistake for food reactions. Hand, foot, and mouth disease, a common viral infection in young children, characteristically produces painful red spots around the mouth, hands, and feet, often accompanied by fever and reduced appetite.
Impetigo, a bacterial skin infection, creates distinctive honey-colored crusty patches that frequently begin around the mouth and nose. Unlike food-related irritation, impetigo is contagious and requires antibiotic treatment.
Roseola and other childhood viral illnesses may produce rashes that include the mouth area as part of a more widespread rash pattern. These infections typically present with additional symptoms like fever, congestion, or general malaise that help distinguish them from simple food reactions.
The timing of infectious rashes differs significantly from food-related irritation. While food irritation appears immediately after exposure, infectious rashes often develop gradually or appear after other symptoms have been present for days.
Underlying skin conditions that affect the mouth area
Eczema and dermatitis conditions can manifest prominently around the mouth, creating ongoing or recurring rash patterns. Perioral dermatitis specifically affects the skin around the mouth, creating red, sometimes scaly patches that may burn or itch. This condition is more common in children who use steroid creams or certain facial products.
Atopic dermatitis, the most common form of eczema, frequently appears in the facial area in children. When it affects the mouth region, it typically creates dry, itchy, and inflamed patches that may crack or weep with increased irritation. Unlike food-related rashes, eczema tends to persist for days or weeks and often recurs in the same locations.
Children with underlying skin conditions may experience flare-ups triggered by food or environmental exposures without having true allergies to these substances. Managing the underlying skin condition through appropriate moisturization and prescribed treatments often reduces these reactive episodes.
Environmental triggers beyond the kitchen
Environmental exposures frequently cause localized reactions around children’s mouths. Bug bites, particularly from mosquitoes, may create raised, itchy welts that can appear anywhere on exposed skin, including around the mouth. Children often inadvertently transfer irritants from their hands to their mouth area after touching plants like poison ivy or household chemicals.
Heat rash can develop in the delicate skin around the mouth, especially in hot, humid weather or when children have been active. This presents as tiny red bumps or blisters and is most common in skin folds and areas where sweat accumulates.
Certain fabrics, metals in jewelry, or chemicals in cosmetic products can trigger contact dermatitis around the mouth. Even seemingly innocuous items like toothpaste ingredients or lip balm components may cause reactions in sensitive children.
These environmental triggers typically produce distinctive patterns based on the exposure type. Parents can often identify the cause by considering recent outdoor activities, new personal care products, or changes in household items.
True food allergies and their distinctive symptoms
Genuine food allergies cause immune-mediated reactions that extend beyond simple skin irritation. When allergic children consume trigger foods, their immune system produces an inappropriate response that can affect multiple body systems. Eight foods account for approximately 90% of all food allergies in children, milk, eggs, peanuts, tree nuts, wheat, soy, fish, and shellfish, with sesame recently recognized as another significant allergen.
True allergic reactions typically develop within minutes to two hours after consuming the allergen. The mouth-area rash in food allergies often presents as raised, intensely itchy hives that may extend beyond the mouth region. Additional symptoms frequently accompany the rash, including:
Swelling of the lips, tongue, or face Gastrointestinal distress including stomach pain, nausea, vomiting, or diarrhea Respiratory symptoms such as sneezing, wheezing, coughing, or difficulty breathing Systemic reactions like dizziness or drops in blood pressure in severe cases
Parents should be particularly vigilant if mouth-area rashes appear in conjunction with these additional symptoms, as this pattern strongly suggests a true food allergy requiring medical evaluation.
Less common causes worth considering
Certain medications and supplements can trigger rashes around the mouth, either through direct contact irritation or systemic allergic responses. Antibiotics, particularly penicillin derivatives, are common culprits for allergic rashes in children. These medication-induced rashes often appear more widespread rather than concentrated solely around the mouth.
Nutritional deficiencies occasionally manifest with perioral rashes. Deficiencies in B vitamins, zinc, or iron can create characteristic skin changes around the mouth. Unlike allergic reactions, these develop gradually and persist until the underlying nutritional issue is addressed.
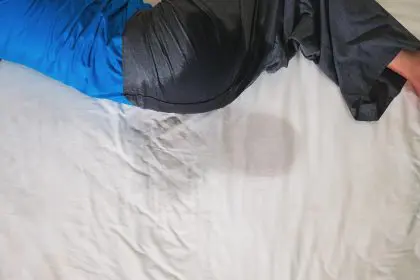
Some children develop perioral rashes in response to excessive drooling or pacifier use. The constant moisture creates an environment conducive to skin irritation and sometimes yeast overgrowth, leading to persistent redness and discomfort.
These less common causes typically require professional evaluation, as they’re difficult to distinguish from other conditions without specialized knowledge and testing.
When to seek immediate medical attention
While many mouth-area rashes resolve with simple home care, certain warning signs demand prompt medical intervention. Parents should seek emergency care if their child experiences:
Difficulty breathing or noisy breathing Swelling of the throat or tongue Severe, widespread hives Significant facial swelling Changes in consciousness or extreme lethargy Persistent vomiting or severe abdominal pain
These symptoms may indicate anaphylaxis, a life-threatening allergic reaction requiring immediate treatment with epinephrine and emergency medical care.
For non-emergency situations, parents should consult a healthcare provider if rashes persist beyond a few days, recur frequently, or cause significant discomfort. Documenting the rash with photos and noting any potential triggers helps medical professionals make accurate diagnoses.
Managing reactions and preventing recurrence
For mild irritant reactions, simple interventions often suffice. Gently washing the affected area with cool water and mild soap removes residual irritants. Applying petroleum jelly or a pediatrician-approved barrier cream protects healing skin and prevents further irritation.
Children with identified food allergies require more comprehensive management strategies. Complete avoidance of allergenic foods becomes essential, necessitating careful label reading and communication with caregivers, schools, and restaurants. For children with severe allergies, carrying emergency medication like epinephrine auto-injectors provides crucial protection against accidental exposures.
Beyond these immediate measures, working with healthcare providers to identify specific triggers through careful observation or formal allergy testing empowers families to prevent future reactions. For persistent or recurrent rashes, dermatologists may recommend specialized skincare regimens or prescription treatments tailored to the underlying cause.
Understanding the diverse causes of mouth-area rashes helps parents respond appropriately to these common childhood occurrences. While many cases resolve easily with minimal intervention, recognizing the warning signs of serious reactions ensures children receive timely medical care when needed. By observing patterns, documenting symptoms, and working closely with healthcare providers, parents can effectively manage these concerning but typically manageable skin conditions.