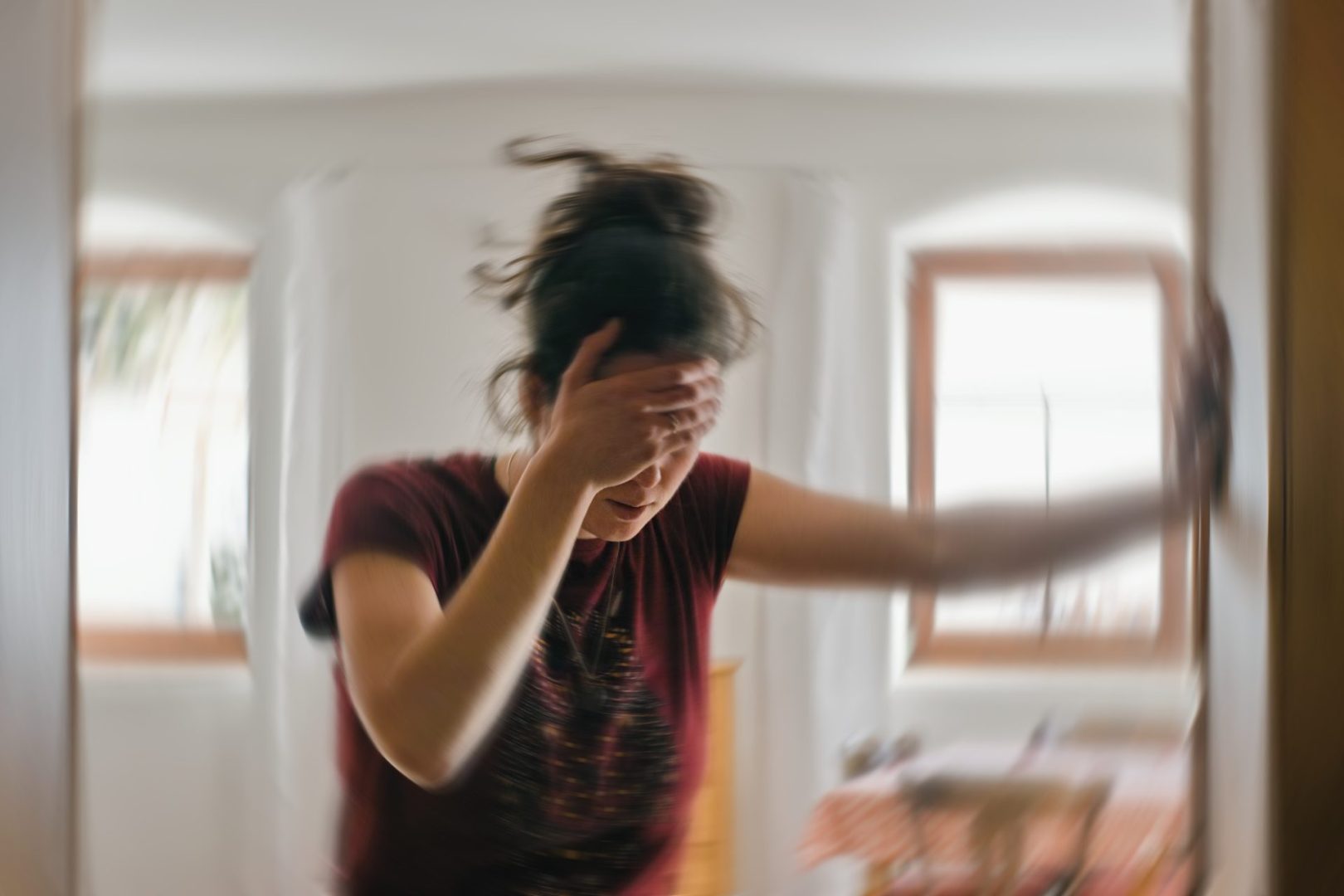
The modern juggling act of careers, relationships, and personal responsibilities creates unprecedented pressure on young adults. Now, a groundbreaking study published in Neurology reveals this chronic stress carries more than just mental health consequences – it significantly increases stroke risk, particularly for women between 18 and 49.
The surprising gender gap in stress-related health risks
The comprehensive research examined 426 individuals who had experienced ischemic strokes alongside an equal number who hadn’t. Participants completed detailed questionnaires about their stress levels during the month before the study. The results revealed a startling pattern: 46% of those who had suffered strokes reported moderate to high stress levels, compared to only 33% of those without stroke history.
Most concerning was the pronounced gender disparity within these findings. Women experiencing moderate stress showed a 78% higher stroke risk, while those reporting high stress levels faced a 6% increase. Meanwhile, researchers found no significant correlation between stress levels and stroke risk among the male participants, raising critical questions about fundamental physiological differences in how stress affects women’s bodies.
This gender disparity demands attention as stroke rates continue rising among younger adults nationwide – a troubling trend that contradicts the traditional understanding of stroke as primarily affecting older populations.
The physiological pathway from stress to stroke
Chronic stress creates a cascade of biological reactions that can damage the cardiovascular system over time. When stress persists without adequate recovery periods, it strains blood vessels, elevates blood pressure, and promotes inflammation throughout the body – all recognized risk factors for stroke.
For women specifically, these stress responses may interact with hormonal fluctuations and other female-specific biological factors to create unique vulnerabilities. The body’s fight-or-flight response, designed to handle short-term threats, becomes chronically activated under persistent stress, leading to vascular changes that increase stroke susceptibility.
Stress can also trigger temporary heart rhythm abnormalities and spikes in blood pressure that may dislodge existing arterial plaques or create conditions where blood clots form more easily. Additionally, many people under chronic stress adopt coping behaviors like smoking, alcohol consumption, poor eating habits, or medication non-adherence – further amplifying their stroke risk.
Why women bear a heavier stress burden
Several factors may explain why women appear more vulnerable to stress-related stroke risk. Modern women often shoulder multiple demanding roles simultaneously – professional obligations, household management, childcare responsibilities, and elder care – creating layers of chronic stress that accumulate over time.
Societal expectations around caregiving and emotional labor also place disproportionate pressure on women. Many feel compelled to maintain a perfect exterior while managing internal stress, potentially creating a disconnect between apparent coping and actual physiological strain.
Healthcare researchers also note potential reporting differences, as women may be more forthcoming about stress experiences while men might minimize or underreport similar symptoms due to cultural expectations around masculinity and emotional expression.
The biological reality of reproductive hormones adds another layer of complexity. Estrogen’s protective cardiovascular effects diminish during high-stress periods, potentially removing a natural safeguard against vascular damage. Birth control, pregnancy history, and menopause transitions further complicate the relationship between stress and cardiovascular health in ways unique to women.
Recognizing when stress becomes dangerous
Identifying stress before it reaches health-damaging levels remains crucial for prevention. The body often sends clear signals that stress has become problematic, including:
Persistent feelings of anxiety or being overwhelmed Disrupted sleep patterns or insomnia Recurring tension headaches Unexplained blood pressure elevations Emotional and physical exhaustion Changes in appetite or weight Difficulty concentrating Digestive issues Muscle tension and unexplained pain
These symptoms warrant attention not merely as quality-of-life issues but as potential warning signs of more serious health consequences developing. Women experiencing multiple stress symptoms should consider them as legitimate health concerns deserving medical attention.
Beyond these chronic stress indicators, everyone should know the warning signs of an actual stroke, which require immediate emergency care:
Sudden numbness or weakness in the face, arm, or leg, especially on one side Unexpected confusion or trouble speaking Visual disturbances affecting one or both eyes Severe headache without known cause Difficulty walking, dizziness, or balance problems
The acronym FAST (Face drooping, Arm weakness, Speech difficulties, Time to call emergency services) provides an essential memory tool for recognizing stroke symptoms when every minute counts.
Effective stress management strategies for protection
While completely eliminating stress remains unrealistic in modern life, developing effective management techniques can significantly reduce its physiological impact. Regular physical activity stands among the most powerful interventions, with research suggesting that 150 minutes of moderate exercise weekly provides substantial stress-reducing benefits.
Mind-body practices offer another evidence-backed approach. Meditation, yoga, and tai chi have demonstrated measurable effects on stress hormone levels and cardiovascular function. Even brief daily mindfulness practices – like focused breathing for ten minutes – can interrupt the stress response cycle and promote recovery.
Social connection plays an equally important protective role. Maintaining strong relationships and having spaces to discuss stressors openly correlates with better stress resilience and reduced cardiovascular risk. For women especially, building support networks that acknowledge their specific challenges can provide both emotional buffering and practical assistance during high-stress periods.
Sleep quality deserves particular attention, as it forms the foundation for stress recovery. Practicing good sleep hygiene – consistent bedtimes, screen-free wind-down periods, and comfortable sleep environments – helps repair the daily damage stress inflicts on the cardiovascular system.
For those experiencing significant stress that feels unmanageable, professional intervention through therapy, counseling, or stress management programs can provide personalized strategies. Cognitive-behavioral approaches have proven particularly effective at breaking chronic stress cycles and teaching sustainable coping skills.
Creating systemic solutions for women’s health
Addressing the disproportionate impact of stress on women’s cardiovascular health requires both individual and societal approaches. Workplaces can implement policies that recognize the full scope of responsibilities many women juggle, including flexible scheduling, family leave, and wellness initiatives specifically addressing stress reduction.
Healthcare providers must incorporate stress assessment into routine care, particularly for younger women who might otherwise be considered low-risk for stroke. This includes asking about stress levels during regular checkups and providing resources before stress-related damage occurs.
Public health initiatives targeting young women should emphasize that stress management isn’t merely about mental wellbeing but represents a legitimate physical health concern. Educational campaigns highlighting the connection between chronic stress and stroke risk could motivate earlier intervention.
Research funding directed toward understanding female-specific cardiovascular risks remains essential. The medical community has historically studied heart disease and stroke primarily in male populations, potentially missing crucial differences in how these conditions develop and manifest in women.
As we continue understanding the complex relationship between stress and stroke risk, particularly among younger women, a dual approach of individual stress management and broader societal support offers the most promising path forward. By recognizing stress as a legitimate health risk rather than merely an emotional state, we can begin addressing this hidden danger before it manifests as life-changing cardiovascular events.