Rolling out: What superpower is required for doctors to treat patients during the COVID pandemic?
Dr. Maya: LOVE!
Everybody’s dealing with trauma. We’re encountering a devastating pandemic that’s invisible. We can’t see it, but it can take our life. There is a mental fall out we experience due to this traumatic reality. The trauma only escalates when that thing doesn’t go away after a period of time.
As healthcare workers, we see this fall out day in and day out, especially since there’s no cure. So healthcare workers must have something else that binds them to the cause.
I cry every morning because of the devastating effect COVID-19 is having, particularly on the people within our community. But then I have to tap into a power greater than the notion of “doing your job.” It’s a marriage to this cause and purpose to fight and not quit. Your heart has to be tied to it!
My heart and love is tied to my community and my goal is to see more of my community on the other side of the pandemic. I truly believe it will come down to an unconditional love for humanity as the superpower that will get us through this.
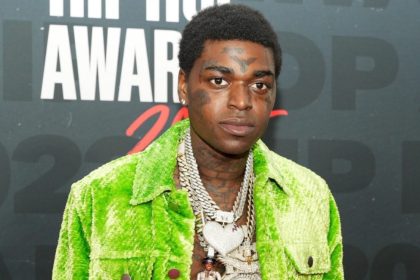
What thoughts and emotions do you have when black patients like the man referenced are denied treatment when its’ obvious their lives were at risk due to COVID?
My heart breaks at a level I can’t even explain.
It’s heartbreaking when I see a man like him smiling during a test and saying “Ohh I feel alright” — when I can clearly see him using his accessory muscles by his rib cage flexing, as he’s trying to keep a smile on his face — because his wife is there and he doesn’t want to put pressure on her. Plus I know it’s nearly impossible for significant others under such turmoil to stay 6 feet apart. Then she gets tested and tests positive for COVID too.
What makes it even more heartbreaking is as a medical professional you see what’s going on and you see the limited options. Whenever the medical community announces there’s a “limited resource,” that is historically code for overlooking our communities. This means our people will have trouble getting it (i.e. tests/vaccines/etc.).
I get angry and disappointed with the healthcare institution for repeatedly doing it. We go through a period of shock and gaslighting. Then we do inherently flawed research, when that’s not needed. We know the industry is biased against Black and Brown communities. It feels like I’m in the Twilight Zone, like the movie Groundhog Day – because this has not only been going on during my lifetime…but since the beginning of this country.
But you know you can’t leave – and you gear yourself up for the fight ahead. We must stay committed to creating a counter-trend to move the system and protect the people we serve, not overlook them.
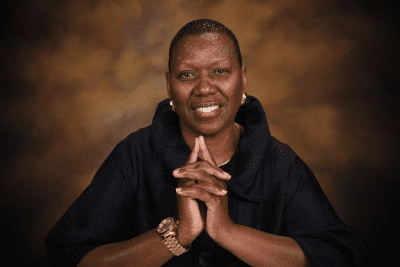
What inspired you to become a doctor that specializes in treating people of color in underserviced communities?
My Mom was my first inspiration. People tell me it must’ve been hard to go to medical school. I respond, “You haven’t met my Mom yet.” She’s the real superhero for creating a situation where I could even imagine becoming a doctor and set out to do it – because she had to deal with so much as a Black mother raising kids on the southside of Chicago.
I remember going to the doctor with my Mom as a child and he would tell her, “Stop smoking.” But he never understood and treated the “why” for her smoking habit.
I knew she was smoking because she was under stress, due to the environment around her. My Mom gave everything so me and my siblings could have a life that shielded us from the environment around her – so we could grow up in a respectable manner. But she smoked as a way of coping with the mental and emotional trauma of trying to raise Black kids in this society.
I realized an annual check-up with a doctor saying, “Hey stop smoking,” wasn’t going to cut it. You have to bring resolution to relieve the trauma she’s trying to escape with that cigarette. Until you address that it’s not going to get us anywhere. I became committed to treating those underlying reasons for those within our community.
I also had an Uncle who died of an AIDS-related pneumonia in the 80s. I remember how my Mom used to breakdown and cry so hard it sounded like she was laughing – after visiting him during his last days. She couldn’t understand why his biological family wouldn’t visit him. She would also notice how doctors talked to him like he deserved to be dying of HIV. It made me realize the humane need to meet patients where they are, removing judgment, and supporting them.
Experiencing this moved me to becoming a doctor that’s equally and unconditionally caring to all people, of all walks of life.