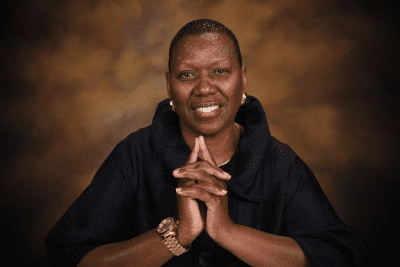
What is your outlook regarding the social work you appear to incorporate within your medical practice?
I’ve learned that any time we see an opportunity to do better – that’s the universe telling us to do it better. I chose to be a doctor to help heal physical, emotional and social wounds in our society that were too often left untreated.
A medical degree was the way to circumvent the social construct & system. What I saw early in the game, was if I became a doctor – I could do the social work and suggest the social solutions with care – which is what I believe are the basics doctors and nurses should be doing anyway.
How were you able to stay strong during this pandemic?
My tribe! I have a dope family that lifts me up energetically. I know they’re always praying for me. My mom will even send me a pie at work – and Lord knows I don’t need the extra calories lol.
I also practice meditation. With everything going on it’s becoming increasingly important for me to find a space to open my space to solutions and pathways to continue to produce for my community at the forefront of access. So I take 10-15 minutes to breathe and open myself up for the next possibility to stay in action for my community.
What was your thought process behind strategically setting up testing tents and the mobile testing regimen for underserviced communities in Chicago?
I wanted to uniquely pull resources into my community to accelerate the care of our people for COVID during this pandemic– to best prevent and slowdown negative outcomes, by circumventing an inherently biased algorithm for determining access to medical resources.
When the city began building out tents for testing at the start of the pandemic, they weren’t built out in an equitable manner, so it didn’t touch the capacity for which we needed it in the Black community.
Plus when you create a shelter in place strategy, we fail to recognize that’s a luxury many of us take for granted. Many in our communities live in a small place not big enough to properly social distance. Also having transportation to go to a testing site, as well as a primary physician to contact to navigate symptoms and treatment, is a luxury. When you create a shelter in place, but don’t give the people the tools to do so, it’s a problem.
So the thought process became “What can I do rapidly?” Well, I decided I can just drive and pull up to our neighborhoods. I can drive to these places, set a schedule, and then people can get access to a test, and hopefully soon the vaccine. Now at senior centers in our community seniors can just take the test right at their door. That’s how you support shelter in place.
When I’m mobile in the van — on the spot I can make a clinical decision to get our people the test on the south and westside of Chicago – using tools I have to bring equity to medicine.
What are your recommendations for people affected by covid?
If you’re impacted by COVID, you have to be alone and quarantine as much as possible for two weeks. People around you should also continue to wear masks, as well as yourself.
Also here are 6 critical tips:
1. At any point you have shortness of breath call 911 (to get supplemental oxygen – do not try to manage alone)
2. Take Vitamin Supplements – Vitamin D (healthy vegetables & fruit)
Stay away from food that slows you down (food that makes you sleepy like steak and beef)
3. Take medicines for chronic illnesses
Ask for 90 days of medication from your doctor – especially if you have chronic conditions
4. Continue to handwash constantly
5. Invest in your mental and spiritual health (mental, spiritual, and physical healing is not separate)
6. Manage symptoms
If symptoms are really bad go to a primary care site for medicine – but if shortness of breath, call 911
– Written by Marcellus L. Womack